Oral microbiota: Roles and treatment in radiation injury (Review)
- Authors:
- Jiaqin Song
- Lei Xia
-
Affiliations: Department of Cancer Center, The Second Affiliated Hospital of Chongqing Medical University, Chongqing Key Laboratory of Immunotherapy, Chongqing 401336, P.R. China - Published online on: August 8, 2025 https://doi.org/10.3892/ol.2025.15218
- Article Number: 472
-
Copyright: © Song et al. This is an open access article distributed under the terms of Creative Commons Attribution License.
This article is mentioned in:
Abstract
 |
 |
 |
|
De Ruysscher D, Niedermann G, Burnet NG, Siva S, Lee AWM and Hegi-Johnson F: Radiotherapy toxicity. Nat Rev Dis Primers. 5:132019. View Article : Google Scholar : PubMed/NCBI | |
|
Zhao Q, Chen Y, Huang W, Zhou H and Zhang W: Drug-microbiota interactions: An emerging priority for precision medicine. Signal Transduct Target Ther. 8:3862023. View Article : Google Scholar : PubMed/NCBI | |
|
Durrant MG and Bhatt AS: Microbiome genome structure drives function. Nat Microbiol. 4:912–913. 2019. View Article : Google Scholar : PubMed/NCBI | |
|
Spencer CN, McQuade JL, Gopalakrishnan V, McCulloch JA, Vetizou M, Cogdill AP, Khan MAW, Zhang X, White MG, Peterson CB, et al: Dietary fiber and probiotics influence the gut microbiome and melanoma immunotherapy response. Science. 374:1632–1640. 2021. View Article : Google Scholar : PubMed/NCBI | |
|
Jin C, Lagoudas GK, Zhao C, Bullman S, Bhutkar A, Hu B, Ameh S, Sandel D, Liang XS, Mazzilli S, et al: Commensal microbiota promote lung cancer development via γδ T cells. Cell. 176:998–1013.e16. 2019. View Article : Google Scholar : PubMed/NCBI | |
|
Pernigoni N, Zagato E, Calcinotto A, Troiani M, Mestre RP, Calì B, Attanasio G, Troisi J, Minini M, Mosole S, et al: Commensal bacteria promote endocrine resistance in prostate cancer through androgen biosynthesis. Science. 374:216–224. 2021. View Article : Google Scholar : PubMed/NCBI | |
|
Sivan A, Corrales L, Hubert N, Williams JB, Aquino-Michaels K, Earley ZM, Benyamin FW, Lei YM, Jabri B, Alegre ML, et al: Commensal Bifidobacterium promotes antitumor immunity and facilitates anti-PD-L1 efficacy. Science. 350:1084–1089. 2015. View Article : Google Scholar : PubMed/NCBI | |
|
Vétizou M, Pitt JM, Daillère R, Lepage P, Waldschmitt N, Flament C, Rusakiewicz S, Routy B, Roberti MP, Duong CP, et al: Anticancer immunotherapy by CTLA-4 blockade relies on the gut microbiota. Science. 350:1079–1084. 2015. View Article : Google Scholar : PubMed/NCBI | |
|
Baker JL, Morton JT, Dinis M, Alverez R, Tran NC, Knight R and Edlund A: Deep metagenomics examines the oral microbiome during dental caries, revealing novel taxa and co-occurrences with host molecules. Genome Res. 31:64–74. 2021. View Article : Google Scholar : PubMed/NCBI | |
|
Di Stefano M, Polizzi A, Santonocito S, Romano A, Lombardi T and Isola G: Impact of oral microbiome in periodontal health and periodontitis: A critical review on prevention and treatment. Int J Mol Sci. 23:51422022. View Article : Google Scholar : PubMed/NCBI | |
|
Irfan M, Delgado RZR and Frias-Lopez J: The oral microbiome and cancer. Front Immunol. 11:5910882020. View Article : Google Scholar : PubMed/NCBI | |
|
Scannapieco FA: Poor oral health in the etiology and prevention of aspiration pneumonia. Clin Geriatr Med. 39:257–271. 2023. View Article : Google Scholar : PubMed/NCBI | |
|
Park SY, Hwang BO, Lim M, Ok SH, Lee SK, Chun KS, Park KK, Hu Y, Chung WY and Song NY: Oral-gut microbiome axis in gastrointestinal disease and cancer. Cancers (Basel). 13:21242021. View Article : Google Scholar : PubMed/NCBI | |
|
Bruno JS, Al-Qadami GH, Laheij AMGA, Bossi P, Fregnani ER and Wardill HR: From pathogenesis to intervention: The importance of the microbiome in oral mucositis. Int J Mol Sci. 24:82742023. View Article : Google Scholar : PubMed/NCBI | |
|
Dominy SS, Lynch C, Ermini F, Benedyk M, Marczyk A, Konradi A, Nguyen M, Haditsch U, Raha D, Griffin C, et al: Porphyromonas gingivalis in Alzheimer's disease brains: Evidence for disease causation and treatment with small-molecule inhibitors. Sci Adv. 5:eaau33332019. View Article : Google Scholar : PubMed/NCBI | |
|
Benedyk M, Mydel PM, Delaleu N, Płaza K, Gawron K, Milewska A, Maresz K, Koziel J, Pyrc K and Potempa J: Gingipains: Critical factors in the development of aspiration pneumonia caused by Porphyromonas gingivalis. J Innate Immun. 8:185–198. 2016. View Article : Google Scholar : PubMed/NCBI | |
|
Vasconcelos RM, Sanfilippo N, Paster BJ, Kerr AR, Li Y, Ramalho L, Queiroz EL, Smith B, Sonis ST and Corby PM: Host-microbiome cross-talk in oral mucositis. J Dent Res. 95:725–733. 2016. View Article : Google Scholar : PubMed/NCBI | |
|
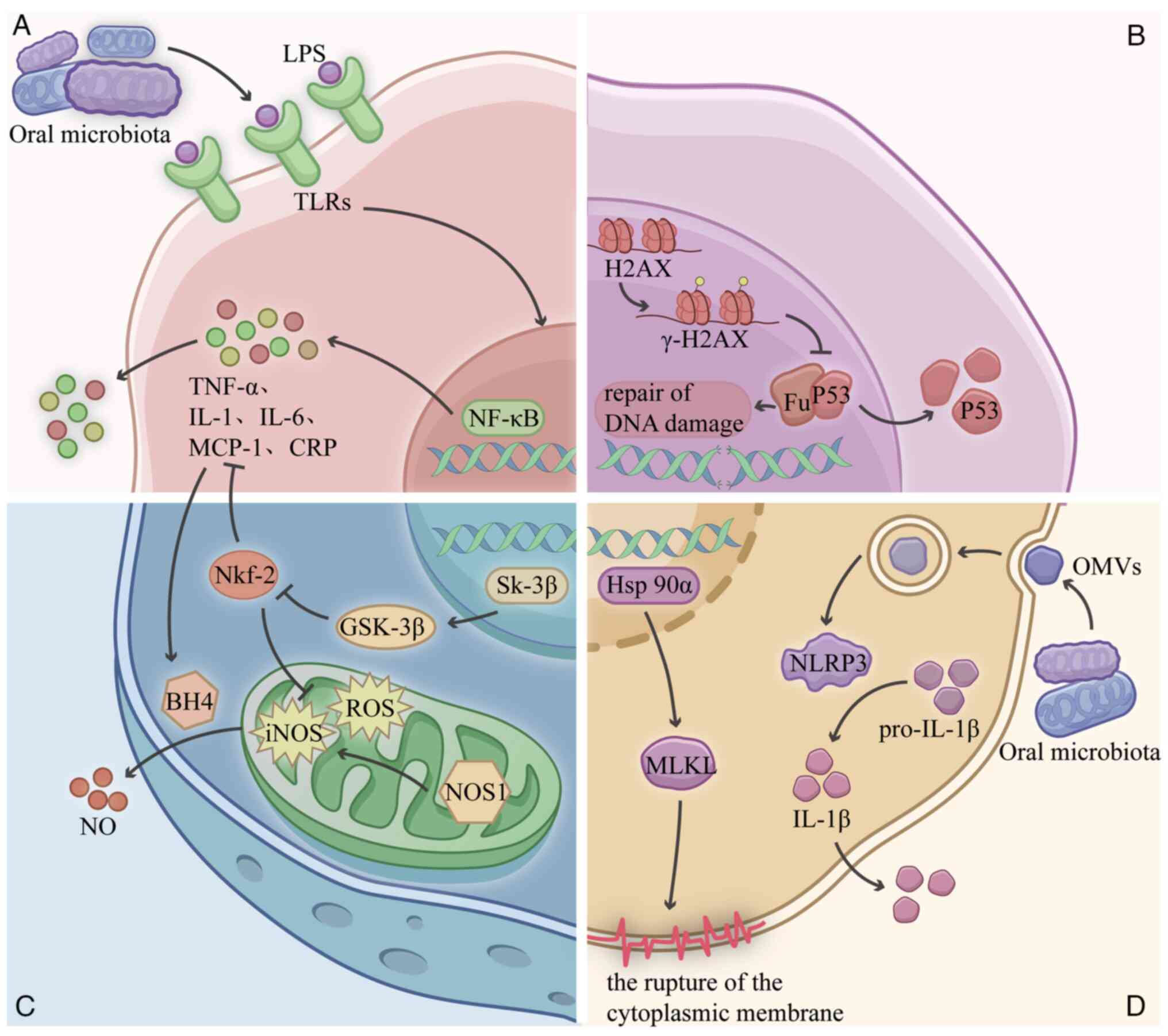
Geng F, Zhang Y, Lu Z, Zhang S and Pan Y: Fusobacterium nucleatum caused DNA damage and promoted cell proliferation by the Ku70/p53 Pathway in oral cancer cells. DNA Cell Biol. 39:144–151. 2020. View Article : Google Scholar : PubMed/NCBI | |
|
Sampath C, Okoro EU, Gipson MJ, Chukkapalli SS, Farmer-Dixon CM and Gangula PR: Porphyromonas gingivalis infection alters Nrf2-phase II enzymes and nitric oxide in primary human aortic endothelial cells. J Periodontol. 92:54–65. 2021. View Article : Google Scholar : PubMed/NCBI | |
|
Feng N, Han X, Peng D, Geng F, Li Q, Pan C, Wang H, Pan Y and Tan L: P. gingivalis alters lung microbiota and aggravates disease severity of COPD rats by up-regulating Hsp90α/MLKL. J Oral Microbiol. 16:23345882024. View Article : Google Scholar : PubMed/NCBI | |
|
Gong T, Chen Q, Mao H, Zhang Y, Ren H, Xu M, Chen H and Yang D: Outer membrane vesicles of Porphyromonas gingivalis trigger NLRP3 inflammasome and induce neuroinflammation, tau phosphorylation, and memory dysfunction in mice. Front Cell Infect Microbiol. 12:9254352022. View Article : Google Scholar : PubMed/NCBI | |
|
Mladenov E, Li F, Zhang L, Klammer H and Iliakis G: Intercellular communication of DNA damage and oxidative status underpin bystander effects. Int J Radiat Biol. 94:719–726. 2018. View Article : Google Scholar : PubMed/NCBI | |
|
Wang K and Tepper JE: Radiation therapy-associated toxicity: Etiology, management, and prevention. CA Cancer J Clin. 71:437–454. 2021.PubMed/NCBI | |
|
Turnquist C, Harris BT and Harris CC: Radiation-induced brain injury: Current concepts and therapeutic strategies targeting neuroinflammation. Neurooncol Adv. 2:vdaa0572020.PubMed/NCBI | |
|
Xu L, Huang H, Liu T, Yang T and Yi X: Exposure to X-rays causes depression-like behaviors in mice via HMGB1-mediated pyroptosis. Neuroscience. 481:99–110. 2022. View Article : Google Scholar : PubMed/NCBI | |
|
Makale MT, McDonald CR, Hattangadi-Gluth JA and Kesari S: Mechanisms of radiotherapy-associated cognitive disability in patients with brain tumours. Nat Rev Neurol. 13:52–64. 2017. View Article : Google Scholar : PubMed/NCBI | |
|
Bowland GB and Weyrich LS: The oral-microbiome-brain axis and neuropsychiatric disorders: An anthropological perspective. Front Psychiatry. 13:8100082022. View Article : Google Scholar : PubMed/NCBI | |
|
Verma A, Azhar G, Patyal P, Zhang W, Zhang X and Wei JY: Proteomic analysis of P. gingivalis-lipopolysaccharide induced neuroinflammation in SH-SY5Y and HMC3 cells. Geroscience. 46:4315–4332. 2024. View Article : Google Scholar : PubMed/NCBI | |
|
Zhang J, Yu C, Zhang X, Chen H, Dong J, Lu W, Song Z and Zhou W: Porphyromonas gingivalis lipopolysaccharide induces cognitive dysfunction, mediated by neuronal inflammation via activation of the TLR4 signaling pathway in C57BL/6 mice. J Neuroinflammation. 15:372018. View Article : Google Scholar : PubMed/NCBI | |
|
Bulgart HR, Neczypor EW, Wold LE and Mackos AR: Microbial involvement in Alzheimer disease development and progression. Mol Neurodegener. 15:422020. View Article : Google Scholar : PubMed/NCBI | |
|
Jin R, Ning X, Liu X, Zhao Y and Ye G: Porphyromonas gingivalis-induced periodontitis could contribute to cognitive impairment in Sprague-Dawley rats via the P38 MAPK signaling pathway. Front Cell Neurosci. 17:11413392023. View Article : Google Scholar : PubMed/NCBI | |
|
Liu Q, Huang Y, Duan M, Yang Q, Ren B and Tang F: Microglia as therapeutic target for radiation-induced brain injury. Int J Mol Sci. 23:82862022. View Article : Google Scholar : PubMed/NCBI | |
|
Wang Y, Tian J, Liu D, Li T, Mao Y and Zhu C: Microglia in radiation-induced brain injury: Cellular and molecular mechanisms and therapeutic potential. CNS Neurosci Ther. 30:e147942024. View Article : Google Scholar : PubMed/NCBI | |
|
Chuang WC, Yang CN, Wang HW, Lin SK, Yu CC, Syu JH, Chiang CP, Shiao YJ and Chen YW: The mechanisms of Porphyromonas gingivalis-derived outer membrane vesicles-induced neurotoxicity and microglia activation. J Dent Sci. 19:1434–1442. 2024. View Article : Google Scholar : PubMed/NCBI | |
|
Maria OM, Eliopoulos N and Muanza T: Radiation-Induced oral mucositis. Front Oncol. 7:892017. View Article : Google Scholar : PubMed/NCBI | |
|
Li J, Zhu C, Zhang Y, Guan C, Wang Q, Ding Y and Hu X: Incidence and risk factors for radiotherapy-induced oral mucositis among patients with nasopharyngeal carcinoma: A meta-analysis. Asian Nurs Res (Korean Soc Nurs Sci). 17:70–82. 2023.PubMed/NCBI | |
|
Nodit L, Kelley JR, Panella TJ, Bruckbauer A, Nodit PG, Shope GA, Peyton K, Klingeman DM, Zaretzki R, Carrell A and Podar M: Oral microbiome and mycobiome dynamics in cancer therapy-induced oral mucositis. Sci Data. 12:4632025. View Article : Google Scholar : PubMed/NCBI | |
|
Hou J, Zheng H, Li P, Liu H, Zhou H and Yang X: Distinct shifts in the oral microbiota are associated with the progression and aggravation of mucositis during radiotherapy. Radiother Oncol. 129:44–51. 2018. View Article : Google Scholar : PubMed/NCBI | |
|
Zhu XX, Yang XJ, Chao YL, Zheng HM, Sheng HF, Liu HY, He Y and Zhou HW: The potential effect of oral microbiota in the prediction of mucositis during radiotherapy for nasopharyngeal carcinoma. EBioMedicine. 18:23–31. 2017. View Article : Google Scholar : PubMed/NCBI | |
|
Vesty A, Gear K, Biswas K, Mackenzie BW, Taylor MW and Douglas RG: Oral microbial influences on oral mucositis during radiotherapy treatment of head and neck cancer. Support Care Cancer. 28:2683–2691. 2020.PubMed/NCBI | |
|
Nishii M, Soutome S, Kawakita A, Yutori H, Iwata E, Akashi M, Hasegawa T, Kojima Y, Funahara M, Umeda M and Komori T: Factors associated with severe oral mucositis and candidiasis in patients undergoing radiotherapy for oral and oropharyngeal carcinomas: A retrospective multicenter study of 326 patients. Support Care Cancer. 28:1069–1075. 2020.PubMed/NCBI | |
|
Groeger S and Meyle J: Oral mucosal epithelial cells. Front Immunol. 10:2082019. View Article : Google Scholar : PubMed/NCBI | |
|
Hirahara L, Takase-Minegishi K, Kirino Y, Iizuka-Iribe Y, Soejima Y, Yoshimi R and Nakajima H: The roles of monocytes and macrophages in Behçet's disease with focus on M1 and M2 polarization. Front Immunol. 13:8522972022. View Article : Google Scholar : PubMed/NCBI | |
|
Suárez LJ, Arboleda S, Angelov N and Arce RM: Oral versus gastrointestinal mucosal immune niches in homeostasis and allostasis. Front Immunol. 12:7052062021. View Article : Google Scholar : PubMed/NCBI | |
|
Li Y, Li Z, Zheng S and Xu X: Probiotics in the management of radiation-induced oral mucositis. Front Cell Infect Microbiol. 14:14771432024. View Article : Google Scholar : PubMed/NCBI | |
|
Zhao M, Wang C, Ji C, Liu R, Xie J, Wang Y and Gu Z: Ascidian-inspired temperature-switchable hydrogels with antioxidant fullerenols for protecting radiation-induced oral mucositis and maintaining the homeostasis of oral microbiota. Small. 19:e22065982023. View Article : Google Scholar : PubMed/NCBI | |
|
Morsy BM, El Domiaty S, Meheissen MAM, Heikal LA, Meheissen MA and Aly NM: Omega-3 nanoemulgel in prevention of radiation-induced oral mucositis and its associated effect on microbiome: A randomized clinical trial. BMC Oral Health. 23:6122023. View Article : Google Scholar : PubMed/NCBI | |
|
Zou XY, Xiang SX and Pan Y: Research advances in traditional Chinese and Western medicine treatments for radiation-induced esophagitis. J Esophagus Dis. 7:129–134. 2025. | |
|
Liu S, Wang S, Zhang N and Li P: The oral microbiome and oral and upper gastrointestinal diseases. J Oral Microbiol. 16:23558232024. View Article : Google Scholar : PubMed/NCBI | |
|
Zou Q, Feng L, Cai X, Qian Y and Xu L: Esophageal microflora in esophageal diseases. Front Cell Infect Microbiol. 13:11457912023. View Article : Google Scholar : PubMed/NCBI | |
|
Yang L, Francois F and Pei Z: Molecular pathways: Pathogenesis and clinical implications of microbiome alteration in esophagitis and Barrett esophagus. Clin Cancer Res. 18:2138–2144. 2012. View Article : Google Scholar : PubMed/NCBI | |
|
Hanania AN, Mainwaring W, Ghebre YT, Hanania NA and Ludwig M: Radiation-induced lung injury: Assessment and management. Chest. 156:150–162. 2019. View Article : Google Scholar : PubMed/NCBI | |
|
Li R, Li J and Zhou X: Lung microbiome: New insights into the pathogenesis of respiratory diseases. Signal Transduct Target Ther. 9:192024. View Article : Google Scholar : PubMed/NCBI | |
|
Pathak JL, Yan Y, Zhang Q, Wang L and Ge L: The role of oral microbiome in respiratory health and diseases. Respir Med. 185:1064752021. View Article : Google Scholar : PubMed/NCBI | |
|
Dong J, Li W, Wang Q, Chen J, Zu Y, Zhou X and Guo Q: Relationships between oral microecosystem and respiratory diseases. Front Mol Biosci. 8:7182222022. View Article : Google Scholar : PubMed/NCBI | |
|
Gaeckle NT, Pragman AA, Pendleton KM, Baldomero AK and Criner GJ: The oral-lung axis: The impact of oral health on lung health. Respir Care. 65:1211–1220. 2020. View Article : Google Scholar : PubMed/NCBI | |
|
Li Q, Wang H, Tan L, Zhang S, Lin L, Tang X and Pan Y: Oral pathogen Fusobacterium nucleatum coaggregates with Pseudomonas aeruginosa to modulate the inflammatory cytotoxicity of pulmonary epithelial cells. Front Cell Infect Microbiol. 11:6439132021. View Article : Google Scholar : PubMed/NCBI | |
|
Takahashi Y, Watanabe N, Kamio N, Yokoe S, Suzuki R, Sato S, Iinuma T and Imai K: Expression of the SARS-CoV-2 Receptor ACE2 and proinflammatory cytokines induced by the periodontopathic bacterium Fusobacterium nucleatum in human respiratory epithelial cells. Int J Mol Sci. 22:13522021. View Article : Google Scholar : PubMed/NCBI | |
|
Suzuki R, Kamio N, Sugimoto K, Maruoka S, Gon Y, Kaneko T, Yonehara Y and Imai K: Periodontopathic bacterium Fusobacterium nucleatum affects matrix metalloproteinase-9 expression in human alveolar epithelial cells and mouse lung. In Vivo. 36:649–656. 2022. View Article : Google Scholar : PubMed/NCBI | |
|
Okabe T, Kamiya Y, Kikuchi T, Goto H, Umemura M, Suzuki Y, Sugita Y, Naiki Y, Hasegawa Y, Hayashi JI, et al: Porphyromonas gingivalis components/secretions synergistically enhance pneumonia caused by Streptococcus pneumoniae in mice. Int J Mol Sci. 22:127042021. View Article : Google Scholar : PubMed/NCBI | |
|
O'Dwyer DN, Kim JS, Ma SF, Ranjan P, Das P, Lipinski JH, Metcalf JD, Falkowski NR, Yow E, Anstrom K, et al: Commensal oral microbiota, disease severity, and mortality in fibrotic lung disease. Am J Respir Crit Care Med. 209:1101–1110. 2024. View Article : Google Scholar : PubMed/NCBI | |
|
Wang Q, Xu G, Yan O, Wang S and Wang X: Radiation-induced injury and the gut microbiota: Insights from a microbial perspective. Therap Adv Gastroenterol. 18:175628482513473472025. View Article : Google Scholar : PubMed/NCBI | |
|
Yamazaki K and Kamada N: Exploring the oral-gut linkage: Interrelationship between oral and systemic diseases. Mucosal Immunol. 17:147–153. 2024. View Article : Google Scholar : PubMed/NCBI | |
|
Wang A, Zhai Z, Ding Y, Wei J, Wei Z and Cao H: The oral-gut microbiome axis in inflammatory bowel disease: From inside to insight. Front Immunol. 15:14300012024. View Article : Google Scholar : PubMed/NCBI | |
|
Yamazaki K: Oral-gut axis as a novel biological mechanism linking periodontal disease and systemic diseases: A review. Jpn Dent Sci Rev. 59:273–280. 2023. View Article : Google Scholar : PubMed/NCBI | |
|
Atarashi K, Suda W, Luo C, Kawaguchi T, Motoo I, Narushima S, Kiguchi Y, Yasuma K, Watanabe E, Tanoue T, et al: Ectopic colonization of oral bacteria in the intestine drives TH1 cell induction and inflammation. Science. 358:359–365. 2017. View Article : Google Scholar : PubMed/NCBI | |
|
Dong J, Li Y, Xiao H, Zhang S, Wang B, Wang H, Li Y, Fan S and Cui M: Oral microbiota affects the efficacy and prognosis of radiotherapy for colorectal cancer in mouse models. Cell Rep. 37:1098862021. View Article : Google Scholar : PubMed/NCBI | |
|
Zou B, Schuster JP, Niu K, Huang Q, Rühle A and Huber PE: Radiotherapy-induced heart disease: A review of the literature. Precis Clin Med. 2:270–282. 2019. View Article : Google Scholar : PubMed/NCBI | |
|
Podlesnikar T, Berlot B, Dolenc J, Goričar K and Marinko T: Radiotherapy-induced cardiotoxicity: The role of multimodality cardiovascular imaging. Front Cardiovasc Med. 9:8877052022. View Article : Google Scholar : PubMed/NCBI | |
|
Liu QH and Liu ZY: Research advances in radiation-induced heart injury. J Microcirc. 34:92–97. 2024. | |
|
Peron D, Prates RA, Antonio EL, Teixeira ILA, de Oliveira HA, Mansano BSDM, Bergamo A, Almeida DR, Dariolli R, Tucci PJF and Serra AJ: A common oral pathogen Porphyromonas gingivalis induces myocarditis in rats. J Clin Periodontol. 49:506–517. 2022. View Article : Google Scholar : PubMed/NCBI | |
|
Bijla M, Saini SK, Pathak AK, Bharadwaj KP, Sukhavasi K, Patil A, Saini D, Yadav R, Singh S, Leeuwenburgh C and Kumar P: Microbiome interactions with different risk factors in development of myocardial infarction. Exp Gerontol. 189:1124092024. View Article : Google Scholar : PubMed/NCBI | |
|
Yang HJ, Zhang Y, Peng O and Zou BW: Radiation-induced heart disease: Current status and challenges. Sichuan Da Xue Xue Bao Yi Xue Ban. 53:1127–1134. 2022.(In Chinese). PubMed/NCBI | |
|
Miyamae N, Ogai K, Kunimitsu M, Fujiwara M, Nagai M, Okamoto S, Okuwa M and Oe M: Relationship between severe radiodermatitis and skin barrier functions in patients with head and neck cancer: A prospective observational study. Asia Pac J Oncol Nurs. 12:1006252024. View Article : Google Scholar : PubMed/NCBI | |
|
Hülpüsch C, Neumann AU, Reiger M, Fischer JC, de Tomassi A, Hammel G, Gülzow C, Fleming M, Dapper H, Mayinger M, et al: Association of skin microbiome dynamics with radiodermatitis in patients with breast cancer. JAMA Oncol. 10:516–521. 2024. View Article : Google Scholar : PubMed/NCBI | |
|
Li W and Yosipovitch G: The role of the microbiome and microbiome-derived metabolites in atopic dermatitis and non-histaminergic itch. Am J Clin Dermatol. 21 (Suppl 1):S44–S50. 2020. View Article : Google Scholar | |
|
Janko M, Ontiveros F, Fitzgerald TJ, Deng A, DeCicco M and Rock KL: IL-1 generated subsequent to radiation-induced tissue injury contributes to the pathogenesis of radiodermatitis. Radiat Res. 178:166–172. 2012. View Article : Google Scholar : PubMed/NCBI | |
|
Curi MM, Cardoso CL, de Lima HG, Kowalski LP and Martins MD: Histopathologic and histomorphometric analysis of irradiation injury in bone and the surrounding soft tissues of the jaws. J Oral Maxillofac Surg. 74:190–199. 2016. View Article : Google Scholar : PubMed/NCBI | |
|
Li Z, Fu R, Huang X, Wen X and Zhang L: Oral microbiota may affect osteoradionecrosis following radiotherapy for head and neck cancer. J Transl Med. 21:3912023. View Article : Google Scholar : PubMed/NCBI | |
|
Hathaway-Schrader JD, Aartun JD, Poulides NA, Kuhn MB, McCormick BE, Chew ME, Huang E, Darveau RP, Westwater C and Novince CM: Commensal oral microbiota induces osteoimmunomodulatory effects separate from systemic microbiome in mice. JCI Insight. 7:e1407382022. View Article : Google Scholar : PubMed/NCBI | |
|
Xu J, Yu L, Ye S, Ye Z, Yang L and Xu X: Oral microbiota-host interaction: The chief culprit of alveolar bone resorption. Front Immunol. 15:12545162024. View Article : Google Scholar : PubMed/NCBI | |
|
Kovtonyuk LV, Caiado F, Garcia-Martin S, Manz EM, Helbling P, Takizawa H, Boettcher S, Al-Shahrour F, Nombela-Arrieta C, Slack E and Manz MG: IL-1 mediates microbiome-induced inflammaging of hematopoietic stem cells in mice. Blood. 139:44–58. 2022. View Article : Google Scholar : PubMed/NCBI | |
|
Klaus R, Niyazi M and Lange-Sperandio B: Radiation-induced kidney toxicity: Molecular and cellular pathogenesis. Radiat Oncol. 16:432021. View Article : Google Scholar : PubMed/NCBI | |
|
Wang WP, Zhang FQ and Yuan SH: Clinical practice guidelines for the prevention and treatment of radiation-induced bladder injury. Chin J Cancer Prev Treat. 30:187–193. 2023. | |
|
Yuan S, Fang C, Leng WD, Wu L, Li BH, Wang XH, Hu H and Zeng XT: Oral microbiota in the oral-genitourinary axis: Identifying periodontitis as a potential risk of genitourinary cancers. Mil Med Res. 8:542021.PubMed/NCBI | |
|
Porter CM, Shrestha E, Peiffer LB and Sfanos KS: The microbiome in prostate inflammation and prostate cancer. Prostate Cancer Prostatic Dis. 21:345–354. 2018. View Article : Google Scholar : PubMed/NCBI | |
|
Prakash P, Verma S and Gupta S: Influence of microbiome in intraprostatic inflammation and prostate cancer. Prostate. 84:1179–1188. 2024. View Article : Google Scholar : PubMed/NCBI | |
|
Wang SY, Cai Y, Hu X, Li F, Qian XH, Xia LY, Gao B, Wu L, Xie WZ, Gu JM, et al: P. gingivalis in oral-prostate axis exacerbates benign prostatic hyperplasia via IL-6/IL-6R pathway. Mil Med Res. 11:302024.PubMed/NCBI | |
|
Liu ZH, Zhou XD and Zhang LL: Research progress in the correlation between oral microbiota and chronic kidney disease. Sichuan Da Xue Xue Bao Yi Xue Ban. 54:66–70. 2023.(In Chinese). PubMed/NCBI | |
|
Kajiwara K, Sawa Y, Fujita T and Tamaoki S: Immunohistochemical study for the expression of leukocyte adhesion molecules, and FGF23 and ACE2 in P. gingivalis LPS-induced diabetic nephropathy. BMC Nephrol. 22:32021. View Article : Google Scholar : PubMed/NCBI | |
|
Zhu W, Zhang X, Yu M, Lin B and Yu C: Radiation-induced liver injury and hepatocyte senescence. Cell Death Discov. 7:2442021. View Article : Google Scholar : PubMed/NCBI | |
|
Acharya C, Sahingur SE and Bajaj JS: Microbiota, cirrhosis, and the emerging oral-gut-liver axis. JCI Insight. 2:e94416–94416. 2017. View Article : Google Scholar : PubMed/NCBI | |
|
Albuquerque-Souza E and Sahingur SE: Periodontitis, chronic liver diseases, and the emerging oral-gut-liver axis. Periodontol 2000. 89:125–141. 2022. View Article : Google Scholar : PubMed/NCBI | |
|
Bai L, Wang YL, Chen YL, Li HX, Zhu SW, Liu Y, Song ZC and Duan SZ: The combination of experimental periodontitis and oral microbiota from periodontitis patients aggravates liver fibrosis in mice. J Clin Periodontol. 49:1067–1078. 2022. View Article : Google Scholar : PubMed/NCBI | |
|
Jia G, Zhi A, Lai PFH, Wang G, Xia Y, Xiong Z, Zhang H, Che N and Ai L: The oral microbiota-a mechanistic role for systemic diseases. Br Dent J. 224:447–455. 2018. View Article : Google Scholar : PubMed/NCBI | |
|
Huang X, Huang X, Huang Y, Zheng J, Lu Y, Mai Z, Zhao X, Cui L and Huang S: The oral microbiome in autoimmune diseases: Friend or foe? J Transl Med. 21:2112023. View Article : Google Scholar : PubMed/NCBI | |
|
Wang Y, Li J, Zhang H, Zheng X, Wang J, Jia X, Peng X, Xie Q, Zou J, Zheng L, et al: Probiotic Streptococcus salivarius K12 alleviates radiation-induced oral mucositis in mice. Front Immunol. 12:6848242021. View Article : Google Scholar : PubMed/NCBI | |
|
De Sanctis V, Belgioia L, Cante D, LA Porta MR, Caspiani O, Guarnaccia R, Argenone A, Muto P, Musio D, DE Felice F, et al: Lactobacillus brevis CD2 for prevention of oral mucositis in patients with head and neck tumors: A multicentric randomized study. Anticancer Res. 39:1935–1942. 2019. View Article : Google Scholar : PubMed/NCBI | |
|
Peng X, Li Z, Pei Y, Zheng S, Liu J, Wang J, Li R and Xu X: Streptococcus salivarius K12 alleviates oral mucositis in patients undergoing radiotherapy for malignant head and neck tumors: A randomized controlled trial. J Clin Oncol. 42:1426–1435. 2024. View Article : Google Scholar : PubMed/NCBI | |
|
Cunha E, Valente S, Nascimento M, Pereira M, Tavares L, Dias R and Oliveira M: Influence of the dental topical application of a nisin-biogel in the oral microbiome of dogs: A pilot study. PeerJ. 9:e116262021. View Article : Google Scholar : PubMed/NCBI | |
|
Wu L, Li F, Ran L, Gao Y, Xie P, Yang J, Ke F, Liu L, Wang Q and Gao X: Insight into the effects of nisin and cecropin on the oral microbial community of rats by high-throughput sequencing. Front Microbiol. 11:10822020. View Article : Google Scholar : PubMed/NCBI | |
|
Gao L, Kuraji R, Zhang MJ, Martinez A, Radaic A, Kamarajan P, Le C, Zhan L, Ye C, Rangé H, et al: Nisin probiotic prevents inflammatory bone loss while promoting reparative proliferation and a healthy microbiome. NPJ Biofilms Microbiomes. 8:452022. View Article : Google Scholar : PubMed/NCBI | |
|
Zhao C, Kuraji R, Ye C, Gao L, Radaic A, Kamarajan P, Taketani Y and Kapila YL: Nisin a probiotic bacteriocin mitigates brain microbiome dysbiosis and Alzheimer's disease-like neuroinflammation triggered by periodontal disease. J Neuroinflammation. 20:2282023. View Article : Google Scholar : PubMed/NCBI | |
|
Nascimento MM: Oral microbiota transplant: A potential new therapy for oral diseases. J Calif Dent Assoc. 45:565–568. 2017.PubMed/NCBI | |
|
Xiao H, Fan Y, Li Y, Dong J, Zhang S, Wang B, Liu J, Liu X, Fan S, Guan J and Cui M: Oral microbiota transplantation fights against head and neck radiotherapy-induced oral mucositis in mice. Comput Struct Biotechnol J. 19:5898–5910. 2021. View Article : Google Scholar : PubMed/NCBI | |
|
Goloshchapov OV, Chukhlovin AB, Bug DS, Polev DE, Kosarev OV, Klementeva RV, Izmailova EA, Kazantsev IV, Khalipskaia MS, Goloshchapova МО, et al: Safety, feasibility, and advantages of oral microbiota transplantation: The first clinical case. J Pediatr Hematol Oncol. 46:287–296. 2024. View Article : Google Scholar : PubMed/NCBI | |
|
AbdelMassih A, Gadalla M, Hussein E, Elahmady M, Zahra N, Eid MA, Hussein M, Hassan AA, Abou-Zeid AS, Hassan A, et al: The forgotten oral microbial transplantation for improving the outcomes of COVID-19. New Microbes New Infect. 43:1009232021. View Article : Google Scholar : PubMed/NCBI | |
|
Zhao F, Huang D and Cao M: Application of bonded medical care peer management model in patients with radiotherapy-induced radiation lung injury for lung cancer. Qilu J Nurs China. 27:19–22. 2021.(In Chinese). View Article : Google Scholar | |
|
Wang N, Wang J and Fang F: Application of 4F nursing management model in patients undergoing radiotherapy for nasopharyngeal carcinoma. Qilu J Nurs China. 29:135–138. 2023.(In Chinese). | |
|
Xiao B, Zou T and Liu Y: Application of 4R crisis management theory in the management of radiation dermatitis in patients with breast cancer during radiotherapy. Mod Med Health. 40:2238–2241. 2024. |










