Bladder leiomyoma in the absence of symptoms: A case report and mini‑review of the literature
- Authors:
- Published online on: May 12, 2025 https://doi.org/10.3892/wasj.2025.350
- Article Number: 62
-
Copyright : © Warli et al. This is an open access article distributed under the terms of Creative Commons Attribution License [CC BY 4.0].
Abstract
Introduction
Mesenchymal tumours are a diverse group of non-epithelial tumours that originate from connective tissue and muscle cells, with bladder leiomyomas representing a subtype. Mesenchymal tumours represent 1-5% of all urinary bladder tumours. Among these, leiomyomas account for 35% and are the most common benign mesenchymal tumours in the bladder (1). Bladder leiomyoma is considered rare, with an incidence rate <0.5% among all types of mesenchymal bladder tumours (2). To date, there are only ~250 case reported worldwide (1-3). Bladder leiomyoma has been reported to be symptomatic more frequently than asymptomatic at the time of the disease being clinically suspected, with a proportion of 83 and 16.8 % cases, respectively (4). Common symptoms reported by patients include lower urinary tract symptoms, haematuria, pyuria and acute urinary retention (4). Some patients have also reported abdominal or back pain which radiates to the left leg (2,4). The diagnosis of bladder leiomyoma is commonly performed using an ultrasound, computed tomography (CT) scan, magnetic resonance imaging (MRI), or cystoscopy (3). The various symptoms and indistinguishable results from several imaging techniques render the diagnosis of bladder leiomyoma challenging.
Given the scarcity of documented cases involving asymptomatic bladder leiomyomas up until the point of treatment, the present study describes the case of a middle-aged female patient who was incidentally diagnosed with asymptomatic bladder leiomyoma during a routine medical check-up. The present case report also emphasizes the importance of long-term follow-up and highlights alternative treatment options for managing bladder leiomyomas.
Case report
A 55-year-old female patient presented for a routine medical check-up at Haji Adam Malik General Hospital, Medan, Sumatera Utara, Indonesia. The overall condition of patient appeared normal, as determined through a comprehensive physical examination, complete blood count (CBC), liver function tests, renal function tests and urinalysis, all of which had values within the normal reference ranges. The patient denied any changes in urinary frequency, dysuria, haematuria, or weight loss over the past year. No issues were reported in bowel movements. The patient denied a history of smoking, familial bladder tumours, bladder stones, urinary tract infections, hypertension, diabetes mellitus, cardiac issues, or previous surgeries.
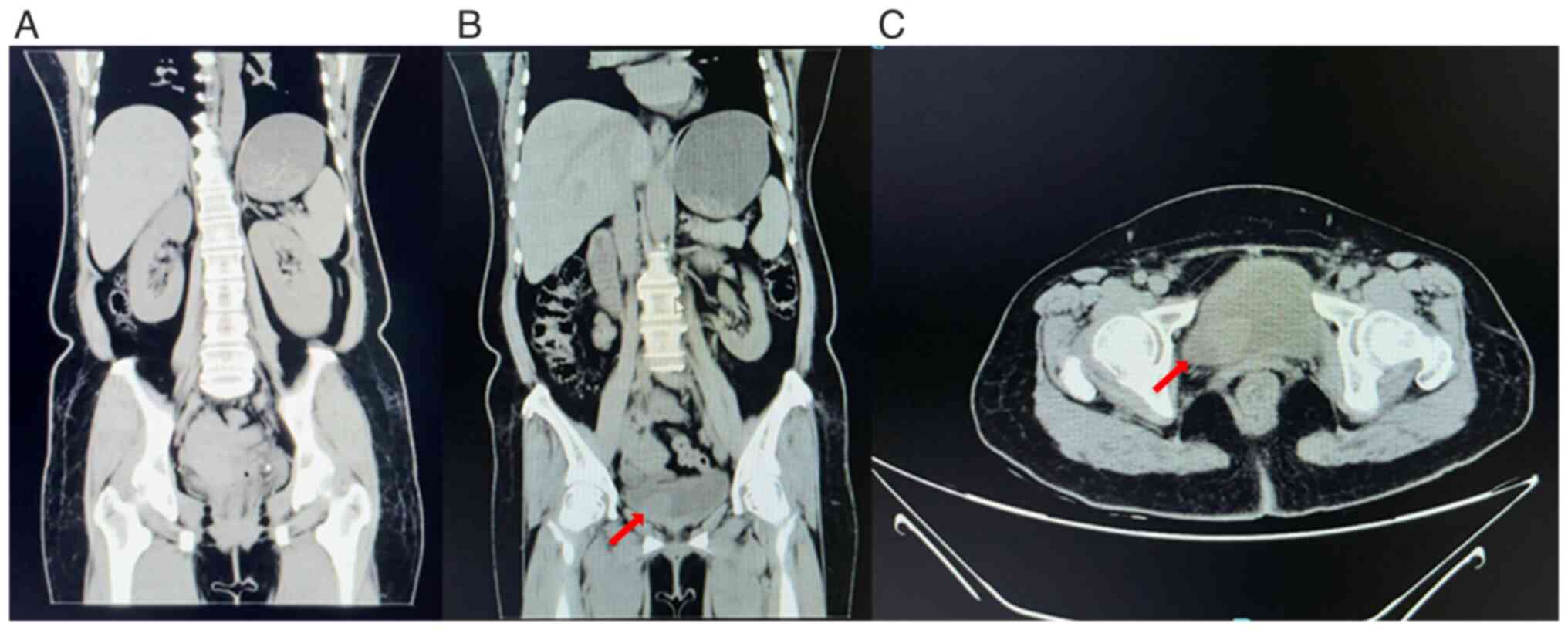
Laboratory investigations revealed a normal results, including a complete blood count (haemoglobin, 13.7 g/dl; leukocytes, 7,310/µl; platelets, 245,000/µl), renal function tests (urea, 43 mg/dl; creatinine, 0.96 mg/dl), liver function tests (AST, 29 U/l; ALT, 32 U/l) and urinalysis (clear appearance, pH 6.0, no protein, glucose, or haematuria detected), all within normal reference ranges. A chest radiography revealed no abnormalities. An abdominal ultrasonography revealed gallstones and a mass within the bladder, suspected of a bladder tumour. Subsequently, a non-contrast CT scan of the entire abdomen was performed, which revealed both kidneys to be within normal limits. An isodense lesion measuring 24x25x21 mm was identified along the right lateral wall of the bladder (Fig. 1).
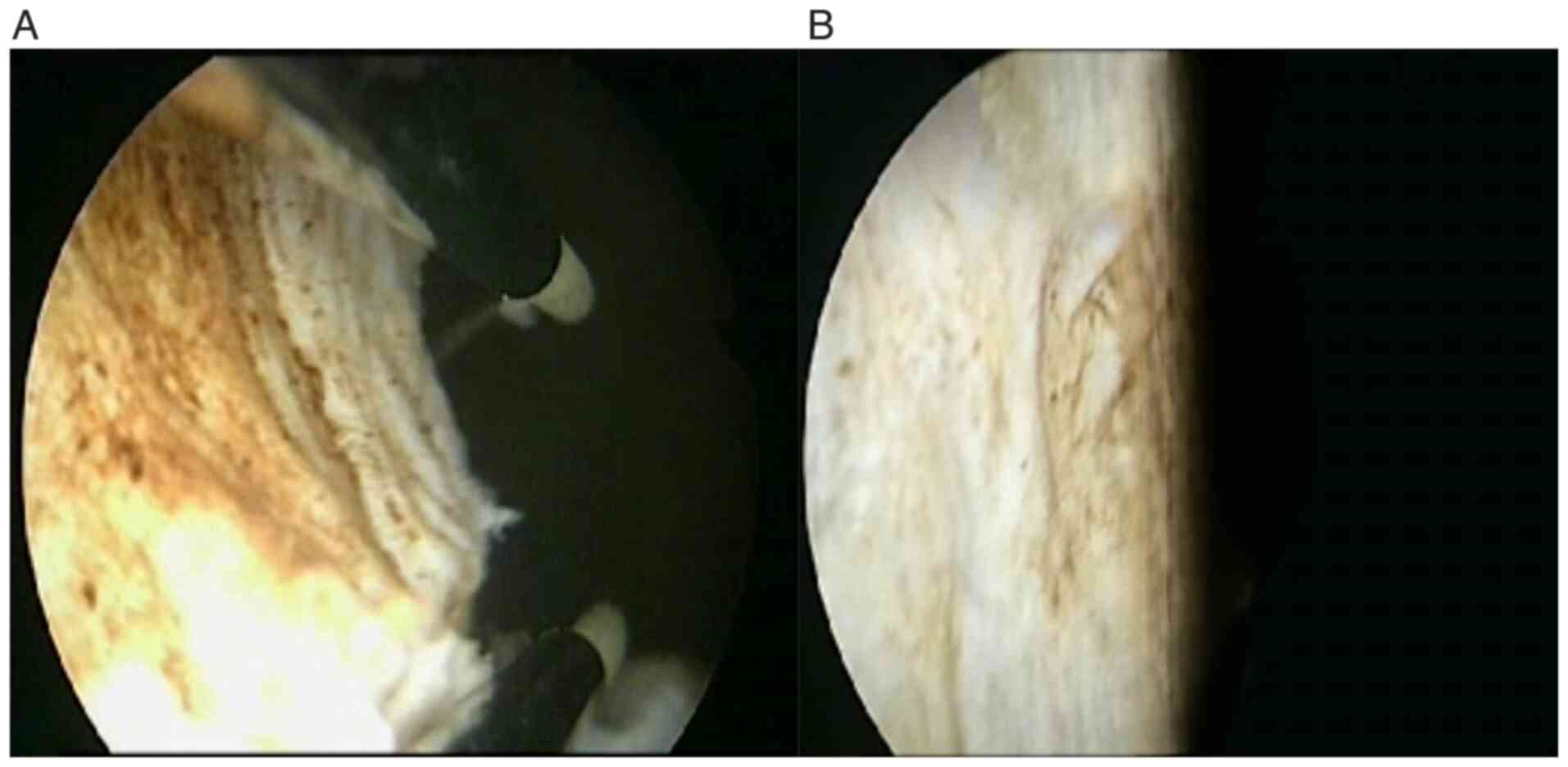
The patient was referred to the Department of Urology at Haji Adam Malik General Hospital, Medan, Sumatera Utara, which revealed inflammatory smears in urine cytology. A cystoscopy was performed, demonstrating non-hyperaemic bladder mucosa, intact ureteral orifices and no trabeculation, vesiculation, or diverticula. A mass was observed on the right lateral aspect of the bladder suspected to be a tumour (Fig. 2). Transurethral resection of the bladder tumour (TURBT) was then agreed upon. TURBT was preferred in account of the tumour size being <3 cm, as it is a procedure with a shorter duration, and is less invasive, therefore improving patient outcomes. No marked bleeding was encountered during the resection procedure, and the tumour was completely excised down to its base (Fig. 3).
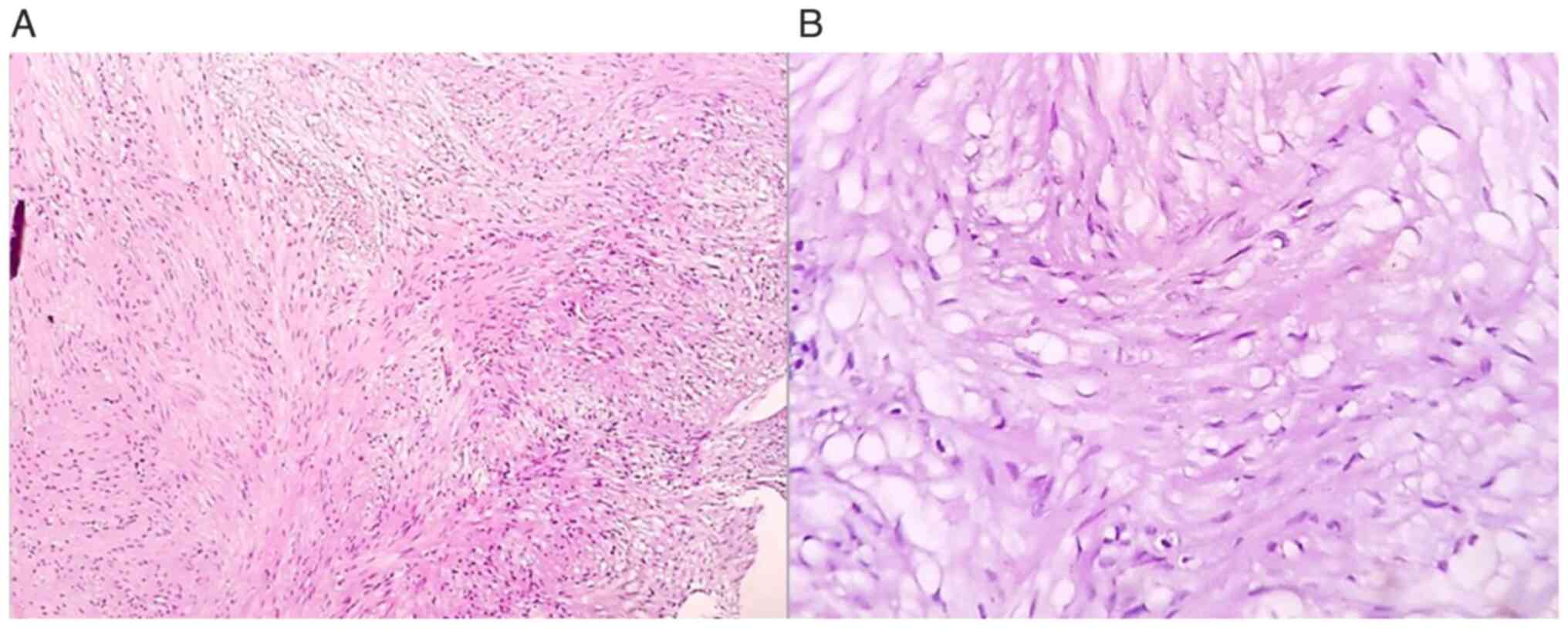
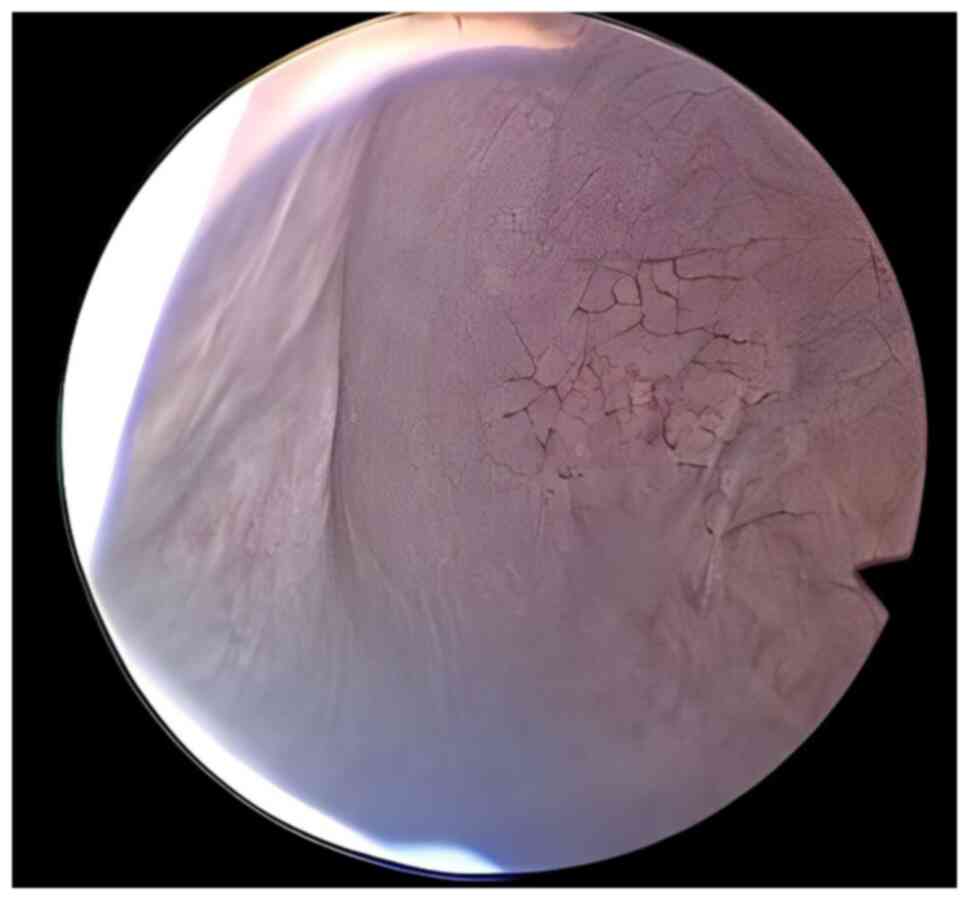
Histopathological analysis of the resected tissue revealed compact interlacing fascicles of smooth muscle cells without significant cytological atypia or mitoses, which confirmed the presence of a bladder leiomyoma (Fig. 4). H&E staining was performed at the Department of Anatomical Pathology, Haji Adam Malik General Hospital, Medan, Indonesia. Tissue sections were 4-µm-thick, formalin-fixed and paraffin-embedded. The specimens were fixed in 10% neutral buffered formalin at room temperature for 24 h. Haematoxylin and eosin staining was conducted using standard protocols with commercially available reagents. Haematoxylin staining utilized Dakewe Biosci Hematoxylin Staining Solution. The stained slides were examined using a light microscope (Olympus CX23, Olympus Corporation). The patient was admitted for 2 days post-operatively without complaints of haematuria or other complications. The patient was immediately discharged upon exhibiting no symptoms. Evaluation was carried out using cystoscopy (Fig. 5) 3 months following TURBT and revealed that there were tumours in the bladder of the patient; the patient also did not have any complaints following TURBT.
Discussion
Leiomyoma of the bladder is an infrequent and benign mesenchymal tumour, accounting for <0.5% of all bladder tumours (1). Initially, it was considered to occur in both sexes at a similar rate; however, subsequent research has revealed that ~70% of cases are found in females. This tumour primarily affects individuals between 30 and 60 years of age, and it typically presents with various symptoms, with obstructive symptoms being the most common (49%), followed by irritative symptoms (38%) and haematuria (11%) (2). Bladder leiomyomas can be classified as endovesical, intramural, or extravesical. Among these, endovesical tumours are the most prevalent and typically manifest with symptoms such as dysuria, urinary urgency, haematuria, and occasionally, lower back pain (3). The aetiology remains unknown as the consequence of its rare incidence. Tobacco smoking, exposure to substances, such as arsenic, radiation, any medications such as opium and chemotherapeutic agents have been reported as significant risk factors for bladder cancer (5). However, to the best of our knowledge, there are no reported risk factors specific to bladder leiomyoma due to its rare incident. Numerous theories have been put forth in an attempt to elucidate the origin of leiomyoma as the consequence of its unknown aetiology. Firstly, Blum's irritative theory posits that chronic inflammatory factors affecting the bladder wall and detrusor smooth muscle may be a contributing factor. Secondly, Piegel's disontogenic theory suggests that these tumours may originate from embryonic remnants of Muller and Wolffian ducts. Lastly, Lips-Chutz's theory proposes that leiomyoma development may be linked to endocrine disturbances, with oestrogen and progesterone playing pivotal roles in this regard (1).
Bladder leiomyomas often present with atypical symptoms, leading to misconceptions and misdiagnoses. Numerous case reports have documented instances where leiomyomas were mistaken for different conditions, including uterine fibroids (6), ureterocele (7,8), febrile urinary tract infections (9) and an enlarged prostate gland (10). However, in a small percentage of cases, similar to the case presented herein, ~19% of bladder leiomyomas are incidentally discovered without causing any noticeable symptoms (2,6).
Typically, patients without symptoms tend to have tumour sizes measuring ≤3 cm. As highlighted in the study by Erdem et al (11), a patient remained asymptomatic until the mass reached 3 cm, underscoring the close association between the symptoms of bladder leiomyoma and the location and size of the tumour (11). Przudzik et al (12) documented 3 cases with tumour diameters <54 mm, most of which were situated away from anatomical openings. Musayev et al (13) also presented an asymptomatic case with similar dimensions (20x25x30 mm) and a minimal amount of surrounding soft tissue, mirroring the characteristics observed in the case in the present study. This similarity supports the accurate asymptomatic diagnosis of the case in the present study (12). Song et al (6) described a case of asymptomatic leiomyoma characterized by only microhaematuria, suggesting the importance of obtaining a thorough medical history of the patient prior to performing any invasive procedures or examinations.
The diagnosis of bladder leiomyomas involves several diagnostic modalities, such as cystoscopy, ultrasonography, CT scans, or MRI; however, the definitive confirmation relies on a histopathological examination (11-13). Cystoscopy findings can help differentiate between intramural and endovesical leiomyomas (11). In terms of diagnostic accuracy for leiomyomas located in the bladder floor, a comparison among intravenous urography (IVU), voiding cysto-urethrogram, transabdominal ultrasonography, CT scans and transvaginal ulstrasound has revealed that transvaginal ulstrasound provides the most precise information regarding the location of the mass and its association with neighbouring organs. Nevertheless, it is worth noting that three-dimensional CT scans and MRI are preferred over ulstrasound for their enhanced assessment of delineation planes and the sites of origin (2).
Radiologically, bladder leiomyomas can be mistakenly identified as various other urinary bladder tumours, cystocele, ureterocele, uterine fibroids and pelvic masses (7). Macroscopically, leiomyomas exhibit well-defined borders and thin capsules, presenting as solid masses with a yellow-coloured sectional surface. Under microscopic examination, leiomyomas consist of intersecting smooth muscle fascicles surrounding vascular structures lined with normal endothelium and arranged as bundles extending in various directions (1). Histological analysis typically reveals the absence of necrosis, cellular atypia, or mitotic activity (8).
MRI, as one of the imaging modalities, is more sensitive compared to CT scan and ultrasonography (USG) in distinguishing leiomyoma with leiomyosarcoma and bladder paraganglioma. Leiomyosarcoma typically presents as large, polypoid masses, usually near the bladder dome. Distinguishing it from a bladder leiomyoma can be challenging, as both lesions often exhibit hypo-intensity on T2-weighted MRI. However, features such as poorly defined borders, invasion into adjacent structures and necrotic areas can help differentiate leiomyosarcoma from leiomyoma. Testing for diffusion restriction also assists in distinguishing bladder leiomyosarcomas from bladder leiomyomas (4). According to Hu et al (14), quantitative MRI can effectively differentiate bladder paraganglioma from bladder leiomyoma by evaluating the signal intensity-ratio on T1-weighted imaging (T1WI) or the ADC value.
The management of leiomyoma primarily involves surgical intervention, with the choice of approach contingent upon factors, such as tumour location, size, and its proximity to the bladder wall. In the majority of instances, the preferred method is transurethral (1-3). Given the benign nature of these lesions, the surgical approach should be as conservative as possible. Available treatment options encompass transurethral resection and open surgical procedures like enucleation or partial cystectomy (1). Similar to the case in the present study, the majority of cases have been successfully managed through TURBT (1,2,6,7,9,15). Nonetheless, in select and exceptional cases, specialized procedures have been developed, such as vaginal resection for bladder leiomyoma. Additionally, minimally invasive techniques, such as laparoscopic cystotomy, robotic extramucosal excision, or transvesical laparoscopy can also be considered as suitable alternatives (1,16). Minimally invasive techniques benefit patients in terms of a shorter duration of hospitalization compared to open surgery approaches (4).
Regular follow-up appointments are crucial in the management of leiomyomas, and it is noteworthy that reoperation rates are relatively low in these cases (12). Previous research has revealed that follow-ups on reported cases have yielded no indications of recurrence even up to 20 years post-surgery, or any malignant transformations (11). Of note, 3 cases of bladder leiomyoma recurrence were reported by Park et al (17) and Yogeeta et al (18); 2 patients underwent repeat TURBT and 1 patient underwent enucleation procedure as tumour recurrence management. There was no report of complications related to the procedures in these cases. Incomplete resection was considered to be the cause of recurrences, considering the fact that the tumours were located near the urethral orifice, causing fear of sphincteric or urethral injury (17,18). Therefore, achieving complete resection has been proven to be an effective and essential approach to prevent recurrence (6,17,18). As previously demonstrated, 3-month follow-ups following TURBT generally show favourable outcomes. In their study, Sodo et al (19) performed a CT scan, USG and peak flow measurements for the follow-up of a patient post-TURBT. At 3 and 9 months, they found negative tumour recurrence and the peak and average flows were 21 and 10 ml/min, respectively. The voided volume was 198 ml at 3 months and at 9 months, this increased at 296 ml (19). In the study by Yoshioka et al (20), a 3 month follow-up examination of a cystoscope-assisted laparoscopic enucleation of a large-sized leiomyoma of the urinary bladder revealed no recurrence. In addition, the studies by He et al (21) and Mitchell et al (22) revealed no recurrence even after at least 6 months of follow-up. However, in the study by Yucel et al (23), the patient had left side and back abdominal pain; thus, a CT scan was performed. The CT scan revealed a tumour formation of 6x3.5 cm extending from the left lateral wall to the anterior wall of the bladder. The CT scan also revealed grade 3 left hydroureteronephrosis. As a result, the patient underwent reoperation. Therefore, despite the mostly satisfying outcome, there also a small chance of tumour recurrence and the need for a reoperation following TURBT (23). This is in line with the case report conducted by Goktug et al (24), where in patients with bladder leiomyoma who underwent TURBT, there was no recurrence with evaluation using cystocopy at 6 months post-operatively.
In conclusion, the present case report highlights the rarity of bladder leiomyoma, a benign mesenchymal bladder tumour. The accurate diagnosis of this condition can be challenging, and it is often mistaken for other urinary bladder tumours or pelvic masses. Diagnostic modalities, including cystoscopy and imaging techniques, aid in confirming the diagnosis; however, a histopathological examination remains the definitive confirmation method. The preferred treatment approach is usually transurethral resection, and in a number of cases, this minimally invasive technique has been successful. The case described herein underscores the importance of sharing case reports to enhance understanding of cases with atypical presentations.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be requested from the corresponding author.
Authors' contributions
SMW, KAWY and CTM are surgeons, and they contributed to data acquisition. SMW, KAWY and CTM wrote the initial draft of the manuscript. SMW provided advice and supervision, and was involved in the revision of the manuscript. MHW assisted in the examination of the patient's specimens. SMW, KAWY, CTM and MHW confirm the authenticity of all the raw data. All authors have read and approved the final manuscript.
Ethics approval and consent to participate
Written informed consent for participation in the present study was obtained from the patient.
Patient consent for publication
Written informed consent for publication for the present case report and all associated images was obtained from the patient.
Competing interests
The authors declare that they have no competing interests.
References
|
Zachariou A, Filiponi M, Dimitriadis F, Kaltsas A and Sofikitis N: Transurethral resection of a bladder trigone leiomyoma: A rare case report. BMC Urol. 20(152)2020.PubMed/NCBI View Article : Google Scholar | |
|
Khater N and Sakr G: Bladder leiomyoma: Presentation, evaluation and treatment. Arab J Urol. 11(54)2013.PubMed/NCBI View Article : Google Scholar | |
|
Mendes JE, Ferreira AV, Coelho SA and Gil C: Bladder leiomyoma. Urol Ann. 9:275–277. 2017.PubMed/NCBI View Article : Google Scholar | |
|
Prihadi JC, Hengky A, Lionardi SK and Haruman SP: Characteristics and outcomes in bladder Leiomyoma management: A systematic review of case reports and case series from the past 20 years. BMC Urol. 24(252)2024.PubMed/NCBI View Article : Google Scholar | |
|
Jubber I, Ong S, Bukavina L, Black PC, Compérat E, Kamat AM, Kiemeney L, Lawrentschuk N, Lerner SP, Meeks JJ, et al: Epidemiology of bladder cancer in 2023: A systematic review of risk factors. Eur Urol. 84:176–190. 2023.PubMed/NCBI View Article : Google Scholar | |
|
Song J, Song H and Kim YW: Recurrent atypical leiomyoma in bladder trigone, confused with uterine fibroids: A case report. World J Clin Cases. 10(10728)2022.PubMed/NCBI View Article : Google Scholar | |
|
AlAmri N, Abdullah H, AlIbrahim F, Eid K and AlShehri M: Imaging findings of atypical leiomyoma of urinary bladder simulating ureterocele. J Surg Case Rep. 2022(rjac256)2022.PubMed/NCBI View Article : Google Scholar | |
|
Grice P, O'Dowd S, Parkinson R and Bazo A: Bladder leiomyoma masquerading as a ureterocele. BMJ Case Rep. 14(242866)2021.PubMed/NCBI View Article : Google Scholar | |
|
Haddad RG and Murshidi MM, Abu Shahin N and Murshidi MM: Leiomyoma of urinary bladder presenting with febrile urinary tract infection: A case report. Int J Surg Case Rep. 27:180–182. 2016.PubMed/NCBI View Article : Google Scholar | |
|
Itam S, Elhage O and Khan MS: Large leiomyoma of the bladder masquerading as an enlarged prostate gland. BMJ Case Rep. 2016(bcr2015212800)2016.PubMed/NCBI View Article : Google Scholar | |
|
Erdem H, Yildirim U, Tekin A, Kayikci A, Uzunlar AK and Sahiner C: Leiomyoma of the urinary bladder in asymptomatic women. Urol Ann. 4:172–174. 2012.PubMed/NCBI View Article : Google Scholar | |
|
Przudzik M, Derkaczew M, Łesiów M and Roslan M: Asymptomatic bladder leiomyoma: A report of three cases treated with minimal invasive techniques and a review of literature. Onco Review. 12:59–64. 2022. | |
|
Musayev J, Bagirov A, Hasanov A and Mammadov E: An asymptomatic intramural leiomyoma of bladder in male patient. Austin J Urol. 1(3)2014. | |
|
Hu X, Wang K, Sun M, Li C, Wang H and Guan J: Quantitative MRI in distinguishing bladder paraganglioma from bladder leiomyoma. Abdom Radiol (NY). 48:1051–1061. 2023.PubMed/NCBI View Article : Google Scholar | |
|
AlHalak R, Alkabbani S, Nasseif H, Oghanna N and Janahi F: Bladder leiomyoma treated with transurethral resection of bladder tumor (TURBT): Case report. Int J Surg Case Rep. 98(107464)2022.PubMed/NCBI View Article : Google Scholar | |
|
Rey Valzacchi GM, Pavan LI, Bourguignon GA, Cortez JP, Ubertazzi EP and Saadi JM: Transvesical laparoscopy for bladder leiomyoma excision: A novel surgical technique. Int Urogynecol J. 32:2543–2544. 2021.PubMed/NCBI View Article : Google Scholar | |
|
Park JW, Jeong BC, Seo SI, Jeon SS, Kwon GY and Lee HM: Leiomyoma of the urinary bladder: A series of nine cases and review of the literature. Urology. 76:1425–1429. 2010.PubMed/NCBI View Article : Google Scholar | |
|
Yogeeta F, Malik Z, Rauf SA, Devi M, Tooba F, Jamalvi SA, Rashid M and Erum H: Recurrent bladder leiomyoma: A case report. J Med Case Rep. 18(173)2024.PubMed/NCBI View Article : Google Scholar | |
|
Sodo M, Spirito L, La Rocca R, Bracale U and Imbimbo C: Partial cystectomy in young male for a urachal tumor masquerading a bladder leiomyoma. Arch Ital Urol Androl. 91:51–52. 2019.PubMed/NCBI View Article : Google Scholar | |
|
Yoshioka T, Kawakita M and Kameoka H: Cystoscope-assisted laparoscopic enucleation of a large progressive bladder leiomyoma. J Endourol Case Rep. 5:120–123. 2019.PubMed/NCBI View Article : Google Scholar | |
|
He L, Li S, Zheng C and Wang C: Rare symptomatic bladder leiomyoma: Case report and literature review. J Int Med Res. 46:1678–1684. 2018.PubMed/NCBI View Article : Google Scholar | |
|
Mitchell K, Barnard J and Luchey A: Locally recurrent leiomyoma of the bladder refractory to visually complete transurethral resection: An indication for cystoprostatectomy. Case Rep Urol. 2019(1086575)2019.PubMed/NCBI View Article : Google Scholar | |
|
Yucel C, Budak S, Kisa E, Celik O and Kozacioglu Z: The rare togetherness of bladder leiomyoma and neurofibromatosis. Case Rep Urol. 2018(2302918)2018.PubMed/NCBI View Article : Google Scholar | |
|
Goktug GH, Ozturk U, Sener NC, Tuygun C, Bakirtas H and Imamoglu AM: Transurethral resection of a bladder leiomyoma: A case report. Can Urol Assoc J. 8:E111–E113. 2014.PubMed/NCBI View Article : Google Scholar |