Factors affecting the quality of life of patients with bronchial asthma (Review)
- Authors:
- Published online on: May 27, 2025 https://doi.org/10.3892/wasj.2025.355
- Article Number: 67
-
Copyright : © Mustafina et al. This is an open access article distributed under the terms of Creative Commons Attribution License [CC BY 4.0].
Abstract
1. Introduction
Asthma remains one of the most prevalent chronic respiratory diseases worldwide, affecting an estimated 262 million individuals and contributing to >455,000 related deaths annually, according to the World Health Organization (WHO) (1,2). While often perceived as a manageable condition, asthma continues to place a significant burden on patients, healthcare systems and societies at large. Suboptimal asthma control persists as a global health challenge, despite the widespread availability of evidence-based guidelines and effective pharmacologic therapies (3,4).
Poor control is strongly associated with increased rates of exacerbations, hospitalizations, missed work or school days, impaired lung function, and, most notably, a profound reduction in quality of life (QoL). Asthma-related limitations in physical activity, frequent hospitalizations and the need for continuous medication contribute to a reduced QoL (5). Moreover, the unpredictable nature of asthma exacerbations creates anxiety among patients, further complicating disease management (6,7).
Epidemiological studies underscore the disturbingly low rates of asthma control worldwide. Mortimer et al (8) emphasized the urgent need to address asthma care disparities in low- and middle-income countries (LMICs), where limited access to essential inhaled corticosteroids (ICS) drives high rates of preventable morbidity and mortality. Current guidelines underestimate the benefits of ICS for patients with mild asthma, leading to widespread over-reliance on short-acting β2-agonists (SABA). The authors propose a unified ICS-formoterol inhaler approach for all asthma severities to improve control and reduce exacerbations. However, poor availability and high costs of these inhalers in LMICs remain major barriers. Mortimer et al (8) called for pragmatic trials to assess the feasibility and cost-effectiveness of such strategies and advocated for a World Health Assembly Resolution to ensure universal access to affordable asthma care.
The Global Asthma Report (GAR), prepared by the Global Asthma Network (GAN), underscores the persistent global burden of asthma, particularly in low- and middle-income countries (LMICs), where access to effective management remains limited (9). Despite recent GAN surveys involving over 450,000 participants, revealing little change in asthma prevalence and severity since the early 2000s, a substantial proportion of children, adolescents, and adults continue to experience poorly controlled symptoms. A key concern is the widespread underuse of inhaled corticosteroids (ICS) and the over-reliance on short-acting β2-agonists (SABA), despite updated international guidelines (GINA 2019) recommending ICS-containing therapy for all asthma severities (10). However, cost barriers to ICS-formoterol inhalers hinder their adoption, particularly in LMICs (11).
Socio-demographic characteristics, including age, sex, level of education and place of residence, significantly affect disease perception, treatment adherence and healthcare accessibility (12,13). Studies suggest that older patients, individuals with a lower educational attainment, and those residing in rural areas experience greater challenges in managing their condition due to limited access to specialized care, lower health literacy and financial constraints (14,15). Sex differences also play a role, with females generally reporting a greater severity of asthma and psychological distress than males, potentially due to hormonal fluctuations and differing healthcare-seeking behaviors (16,17).
A critical factor contributing to inadequate asthma control is poor adherence to maintenance therapy. Population-based studies in the USA, Europe and Australia have consistently reported that only 30-50% of patients adhere to prescribed inhaled corticosteroids (ICS), the cornerstone of long-term asthma management (18). Factors such as medication costs, complexity of treatment regimens, fear of side-effects and insufficient patient education all contribute to this shortfall. Moreover, in certain countries, the overuse of short-acting beta-agonists continues to prevail, reinforcing a reactive rather than proactive approach to disease management (19).
Perhaps most striking are the international disparities in achieving optimal asthma control. Countries such as Finland, Sweden and Canada, where national asthma programs have integrated guideline-based care with strong patient education and access to medications, have witnessed marked reductions in hospitalizations, mortality and symptom burden (20,21). By contrast, several nations across Eastern Europe, Latin America, Asia and sub-Saharan Africa continue to report high rates of uncontrolled asthma due to limited access to essential medications, insufficient primary care infrastructure, diagnostic delays and the lack of patient-centered education strategies (22). These disparities are reflected in large variations in health-related QoL (HRQoL) among patients with asthma, with those in resource-constrained settings reporting significantly lower scores across physical, emotional and functional domains (23,24).
Environmental factors are among the most significant contributors to asthma exacerbations and disease progression. Air pollution, allergens, climate variability and occupational exposures all play a role in worsening asthma symptoms. Exposure to fine particulate matter (PM2.5), nitrogen dioxide (NO2), sulfur dioxide (SO2), and ozone (O3) has been strongly linked to airway inflammation, increased bronchial hyper-reactivity and reduced lung function (25,26).
The burden of uncontrolled asthma on QoL is profound and multi-dimensional. Beyond physical symptoms, patients often experience anxiety, depression, social isolation and limitations in personal, professional and academic pursuits. This indicates that asthma is not merely a biomedical condition, but a psychosocial one, demanding a more comprehensive understanding of the interplay between clinical, behavioral, environmental and systemic factors.
Given this urgent and multifaceted global challenge, the present review aimed to synthesize the findings from existing literature on the factors that influence the QoL in patients with asthma. The objective was to identify key determinants that can guide clinicians, researchers and policymakers in developing targeted interventions and healthcare strategies to improve asthma control and ultimately enhance patient well-being (5).
2. Socio-demographic factors
Socio-demographic factors play a crucial role in shaping the QoL of patients with bronchial asthma, influencing disease perception, treatment adherence and overall health outcomes. Among these, age, sex, educational attainment, ethnicity and place of residence are key determinants that affect both the progression of the disease and the effectiveness of asthma management strategies. Understanding these factors can help develop targeted interventions to improve asthma care and patient well-being.
Age is a key determinant of health outcomes in patients with asthma (27). Studies have indicated that younger patients often experience different challenges compared to older individuals (28,29). Children diagnosed with asthma often face a higher risk of hospital readmissions, recurrent exacerbations and long-term lung function decline. Pediatric asthma is commonly triggered by respiratory infections, allergens and environmental pollutants, necessitating a comprehensive approach that includes caregiver education and early intervention. Adolescents, on the other hand, may struggle with treatment adherence due to psychological factors, social influences, or a desire for independence, increasing the likelihood of uncontrolled asthma. In adults, asthma is often associated with occupational exposures, lifestyle factors, and comorbidities such as obesity and cardiovascular disease, which can further complicate disease management. Among the elderly, age-related decline in lung function, polypharmacy and reduced access to healthcare may contribute to poorer disease control and increased morbidity.
Sex differences also play a crucial role in the prevalence and management of asthma (Table I) (30,31). Research suggests that asthma is more common among boys than girls during childhood, although this trend reverses in adulthood, with a higher prevalence among women (32). Hormonal fluctuations, particularly those associated with puberty, pregnancy and menopause, may play a role in modulating airway inflammation and asthma severity (33). Additionally, women often report more severe symptoms, increased healthcare utilization, and a higher likelihood of anxiety and depression, which can further affect their QoL. Social and behavioral factors, such as differences in healthcare-seeking behavior and medication adherence, may also contribute to sex disparities in asthma outcomes (33).
Table ISocio-demographic factors affecting the QoL of patients with asthma, as summarized in the present review. |
Socio-demographic factors, particularly socioeconomic status (SES), play a critical role in shaping asthma-related health outcomes and the QoL of patients (34,35). A lower SES often characterized by limited income, low educational attainment, unstable employment and poor living conditions has repeatedly been found to be associated with poorer asthma control, increased disease burden, and a substantially reduced HRQoL (34,35).
Patients with asthma from disadvantaged socioeconomic backgrounds face multiple, interlocking barriers to achieving good disease management (36). These include reduced access to healthcare services, under-diagnosis, poor continuity of care, limited affordability of essential medications and greater exposure to environmental triggers. Consequently, SES is often not merely a background variable, but a central determinant of both clinical outcomes and psychosocial functioning (36).
Adding further relevance to the current context is a recent population-based study from Kazakhstan by Vinnikov et al (37). Their study, which used the EQ-5D instrument to assess HRQoL, found that age, sex, region of residence, income, education and occupational group were all significantly associated with QoL in the general population. Particularly striking was the finding that respondents with lower income and educational levels consistently reported poorer HRQoL scores mirroring international patterns. That study highlighted the social gradient in health within Kazakhstan and provides a compelling rationale for examining how these socioeconomic disparities influence asthma outcomes specifically (37).
This body of evidence reinforces the conclusion that HRQoL in asthma is not determined solely by disease severity or treatment modality, but is profoundly shaped by the broader socio-economic environment in which the patient lives. Patients with comparable clinical profiles may experience vast differences in QoL depending on their material circumstances, access to care and level of social support.
From a public health perspective, this implies that improving asthma-related QoL requires more than medical intervention. Addressing SES-related disparities, through policies promoting universal health coverage, education, poverty alleviation and housing improvements, is essential for achieving equitable outcomes. In Kazakhstan and other middle-income countries undergoing healthcare reform, these findings underscore the urgency of integrating social determinants of health into asthma care strategies and quality improvement initiatives.
Educational attainment is another critical factor affecting asthma management and QoL. Individuals with lower education levels often lack essential knowledge about their condition, leading to poor self-management, inadequate symptom recognition and reduced adherence to prescribed therapies (38,39). A low health literacy is associated with higher rates of emergency department visits, increased hospitalizations and a greater reliance on short-term relief medications instead of long-term controller therapies. Conversely, patients with higher education levels are more likely to understand the importance of asthma action plans, inhaler techniques and environmental triggers, leading to better disease control and improved QoL (38,39). Targeted patient education programs and simplified treatment instructions can help bridge this gap, ensuring equitable asthma management across different educational backgrounds.
Ethnicity is another critical factor affecting asthma prevalence and treatment outcomes (40,41). Genetic predisposition, environmental exposures, healthcare access and cultural beliefs about disease management all contribute to disparities in asthma care among different ethnic groups. In a number of regions, ethnic minorities face a higher burden of asthma due to socio-economic disadvantages, increased exposure to urban pollution and limited access to healthcare services. Language barriers and mistrust in the healthcare system may further hinder effective communication between patients and providers, resulting in under-diagnosis and suboptimal treatment adherence. Addressing these disparities requires culturally tailored asthma education, improved healthcare accessibility, and community outreach programs to ensure that all ethnic groups receive adequate disease management support.
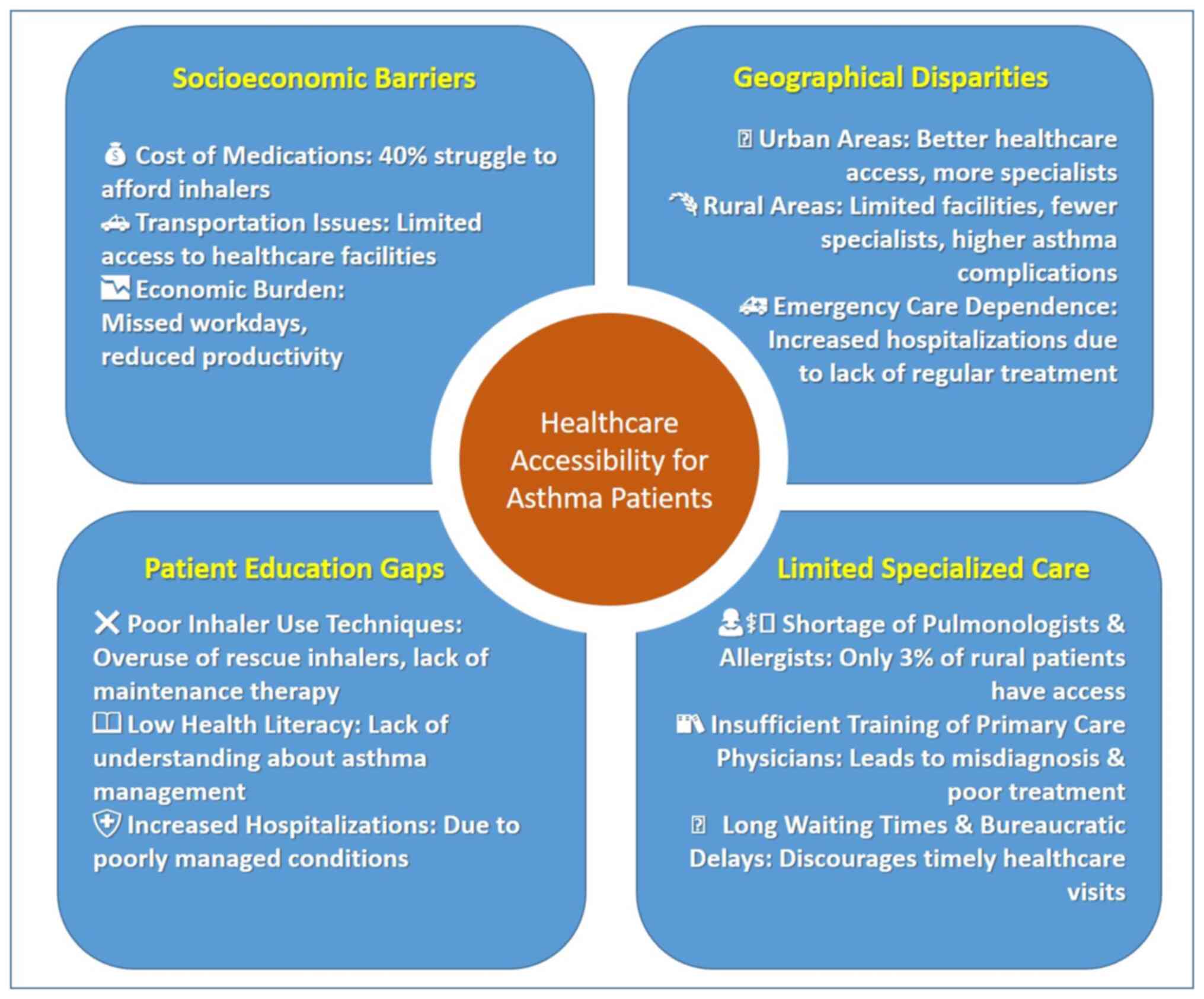
Apart from that, the place of residence (urban vs. rural areas) markedly affects the prevalence and management of asthma (Fig. 1). Urban environments expose individuals to higher levels of air pollution, allergens and occupational irritants, which can exacerbate the symptoms of asthma and lead to increased hospitalizations. However, urban residents typically have better access to healthcare facilities, specialist consultations and advanced treatment options, improving their ability to manage the disease effectively (42). By contrast, rural populations often face limited access to specialized asthma care, diagnostic facilities and essential medications, leading to underreporting, delayed diagnosis and poorer disease control (43). Additionally, rural healthcare providers may lack sufficient training in asthma management, further contributing to disparities in treatment quality. Expanding telemedicine services, increasing healthcare infrastructure in rural areas, and providing ongoing medical education for primary care physicians could help mitigate these challenges and improve asthma outcomes in underserved populations (44).
Socio-demographic factors, such as age, sex, education level, ethnicity and place of residence play a crucial role in determining the QoL of patients with bronchial asthma. Addressing these disparities through targeted public health initiatives, educational programs and healthcare policy improvements could lead to more effective asthma management and better overall health outcomes (44). A patient-centered approach that considers these socio-demographic determinants will be essential in reducing asthma-related morbidity and improving QoL for all affected individuals.
3. Clinical factors
Clinical factors significantly affect the QoL of patients with bronchial asthma, encompassing disease severity, the presence of comorbidities, treatment adherence and the frequency of exacerbations (45). Among the key contributors are disease severity, presence of comorbidities, treatment adherence, frequency of exacerbations and modifiable risk factors, such as smoking status. A comprehensive understanding of these factors is essential for optimizing asthma management and improving patient outcomes.
Disease severity is a primary determinant of QoL, with patients experiencing more severe asthma reporting higher levels of physical and emotional distress. Severe asthma is often characterized by persistent symptoms, frequent exacerbations, and a greater reliance on high-dose corticosteroids and biologic therapies (46). Individuals with uncontrolled asthma face limitations in daily activities, including reduced physical exercise capacity, work productivity and social participation, all of which contribute to lower QoL scores. Research has indicated that patients with severe persistent asthma report a significantly higher number of hospitalizations, emergency room visits and higher healthcare costs than those with mild or moderate disease (47). Early and effective intervention to control inflammation and minimize symptom burden is essential for improving the outcomes of these patients.
The inflammatory mechanisms in asthma-chronic obstructive pulmonary disease (COPD) overlap syndrome (ACOS) involve a complex interplay of both Th2-high inflammation (48), typical of asthma, and neutrophilic inflammation, more commonly observed in COPD (49,50). This combination results in a more severe and less steroid-responsive form of airway disease.
The levels of interleukin (IL)-17) are significantly elevated in ACOS and play a crucial role in driving neutrophilic inflammation (51,52). IL-17 It promotes the recruitment and activation of neutrophils in the airways, leading to increased mucus production, airway remodeling and heightened bronchial hyper-reactivity (53). The increased presence of neutrophils contributes to the persistent airflow limitation characteristic of ACOS.
Tumor necrosis factor-α (TNF-α) is a pro-inflammatory cytokine, the levels of which are upregulated in both asthma and COPD, although its role may be more prominent in COPD and ACOS (54). TNF-α contributes to airway inflammation, mucus hypersecretion and the activation of other inflammatory cells (55). It also promotes the production of matrix metalloproteinases, which are involved in the destruction of lung tissue and the development of emphysema, a common feature in COPD.
An imbalance between oxidants and antioxidants leads to increased oxidative stress in ACOS (56,57). This oxidative stress exacerbates inflammation, impairs corticosteroid responsiveness and contributes to airway damage (58,59). Reactive oxygen species can directly damage lung cells and activate inflammatory pathways, further perpetuating the inflammatory cycle. Additionally, oxidative stress can modify proteins, leading to the formation of neoantigens that may drive autoimmune responses (58,59).
Beyond adaptive immunity, the innate immune system plays a critical role in ACOS. Pattern recognition receptors, such as Toll-like receptors are activated by pathogen-associated molecular patterns and damage-associated molecular patterns, leading to the release of pro-inflammatory cytokines and chemokines (60-62). This activation contributes to the chronic inflammation and airway remodeling observed in ACOS.
Structural cells, such as epithelial cells and smooth muscle cells also contribute to the inflammatory process in ACOS. Epithelial cells release inflammatory mediators in response to injury or stress, while smooth muscle cells can proliferate and contribute to airway thickening. Interactions between structural and immune cells further amplify the inflammatory response (63,64).
In fact, comorbidities play a crucial role in asthma management and patient well-being [2024 Summary Guide for Asthma Management and Prevention, GINA 2024(65)]. The presence of these comorbid conditions complicates asthma management, as they can exacerbate symptoms and increase the frequency of exacerbations. For instance, patients with both asthma and COPD report more severe respiratory symptoms and higher rates of hospitalizations compared to those with asthma alone (66). Patients with coexisting COPD and asthma, commonly referred to as ACOS, tend to experience more severe airflow limitation, increased inflammation and a higher risk of exacerbations, necessitating a multidisciplinary approach to treatment. Similarly, obesity has been linked to greater asthma severity, poorer response to corticosteroids and increased systemic inflammation, further reducing QoL. Addressing comorbidities through tailored treatment plans, weight management strategies and mental health support can lead to more effective disease control and improved patient well-being (65).
Treatment adherence is another critical factor influencing the QoL of patients with asthma. Research indicates that numerous patients do not adhere to prescribed treatment regimens, often due to a lack of understanding about their condition or the importance of consistent medication use (67,68). A previous study found that only a fraction of patients utilized inhaled corticosteroids as recommended, which are essential for controlling inflammation in chronic asthma (69). Poor adherence to treatment not only leads to worse disease control, but also results in increased healthcare utilization, including emergency visits and hospital admissions. Consequently, enhancing patient education regarding the importance of adherence to prescribed therapies is vital for improving overall health outcomes.
The frequency and severity of asthma exacerbations are also closely linked to QoL (70,71). Asthma exacerbations can lead to significant disruptions in daily life, including missed work or school days and limitations in physical activities (7,72). Another study highlighted that patients who experienced frequent exacerbations reported significantly lower QoL scores across various domains, including emotional well-being and activity limitation (73). Specifically, each exacerbation was associated with a decrease in QoL scores, indicating that effective management strategies aimed at reducing exacerbation rates could substantially improve patient experiences (72,74,75). Reducing the frequency of exacerbations through personalized treatment plans, allergen avoidance strategies and a more stringent adherence to medication could significantly enhance the long-term health outcomes of patients.
Moreover, smoking status has been identified as a modifiable risk factor affecting the QoL of patients with asthma (76-78). Active smokers tend to have a significantly lower QoL compared to non-smokers, due to increased symptom severity and exacerbation frequency (79). Smoking cessation programs tailored for asthmatic patients could therefore be beneficial in improving their overall health outcomes (80). A previous study found that smokers with asthma had a significantly higher healthcare utilization and more frequent hospital visits than non-smokers (81). Implementing smoking cessation programs tailored to asthma patients, combined with behavioral counselling and pharmacologic support, could improve lung function, reduce exacerbations and enhance overall health status (82).
To summarize, clinical factors, such as disease severity, comorbidities, treatment adherence and exacerbation frequency play a pivotal role in determining the QoL of patients with asthma. Addressing these factors through targeted interventions, such as enhancing patient education on medication adherence, implementing regular follow-up care for comorbid conditions, and promoting smoking cessation could lead to more effective management strategies and better health outcomes for individuals living with asthma. As highlighted by recent studies, urgent action is required to develop comprehensive care programs that prioritize both pharmacological treatment and holistic patient support to enhance the QoL for asthmatic patients across Kazakhstan (83-85).
4. Environmental factors
Environmental factors play a fundamental role in shaping the QoL of patients with bronchial asthma, influencing disease severity, exacerbation frequency and overall health outcomes. While asthma is a chronic inflammatory condition with a strong genetic component, exposure to environmental triggers can significantly worsen symptoms, increase the frequency of hospitalizations and impair daily functioning. Poor air quality, exposure to allergens, climate variability, occupational hazards and socioeconomic conditions all contribute to the disease burden (Table II). Understanding and addressing these environmental influences is crucial for improving asthma management and enhancing patient well-being.
Air pollution is one of the most critical environmental risk factors for asthma, particularly in urban areas where vehicle emissions, industrial pollutants and biomass combustion are prevalent. PM2.5, NO2, SO2 and O3 contribute to airway inflammation, bronchial hyperresponsiveness and increased asthma exacerbations (86,87). Studies have shown that individuals residing in highly polluted areas, particularly near busy roads or industrial zones, have worse symptom control and a lower QoL compared to those residing in less polluted environments (88,89). Long-term exposure to these pollutants has been linked to reduced lung function, an increased use of medications and a higher risk of emergency hospital visits. Indoor air pollution also plays a crucial role in asthma severity. Sources such as tobacco smoke, cooking fumes, mold spores and volatile organic compounds (VOCs) from household products can worsen respiratory symptoms. Children and the elderly are particularly vulnerable, as their respiratory systems are more sensitive to environmental irritants (90-92). Effective strategies to mitigate the impact of air pollution on patients with asthma include stricter air quality regulations, improved urban planning, reduced reliance on fossil fuels, and promoting cleaner indoor air through ventilation systems, air purifiers and smoke-free policies.
In a number of developing and transition countries, indoor air pollution poses a serious and urgent public health concern, particularly in relation to chronic respiratory diseases, such as asthma. While outdoor (ambient) air pollution has been widely studied, the indoor environment, where individuals spend the majority of their time often remains a neglected source of harmful exposure, particularly in low- and middle-income countries (LMICs). Numerous studies have shown that exposure to indoor pollutants, such as biomass smoke, PM2.5, VOCs, mold and household chemicals, can significantly worsen asthma symptoms, impair disease control and reduce HRQoL (93-95).
There are high levels of both ambient and indoor air pollution found in large urban centers in developing countries (96). These exposures have been causally linked to an increased prevalence of asthma, more frequent exacerbations and greater healthcare utilization. In such settings, indoor air quality is frequently compromised by substandard housing, overcrowding, the use of solid fuels for cooking and heating, and limited ventilation, factors that disproportionately affect socioeconomically disadvantaged groups (97,98) (Table II).
A recent systematic review by Agache et al (99), conducted for the EAACI guidelines, evaluated the impact of indoor exposures, including VOCs, cleaning agents, mold/dampness and pesticides, on the incidence and severity of asthma. Among 94 studies reviewed, exposure to damp and mold had the strongest association with new-onset wheeze (moderate certainty), while cleaning agents, VOCs, and pesticides showed weaker but suggestive links with asthma onset and worsened symptoms. Although the certainty of evidence varied, the findings highlight the broad and cumulative risk posed by multiple indoor pollutants. The authors of that study emphasized the urgent need for more rigorous longitudinal studies to better establish causal associations and inform prevention guidelines (99).
Adding to this evidence, a real-world study in Chicago performed by Kang et al (100) evaluated indoor and outdoor air quality in 41 homes over period of 1 year. Using cross-sectional and longitudinal models, they found that higher indoor concentrations of NO2, PM1, PM2.5 and PM10, as well as elevated indoor temperature and visible mold, were significantly associated with lower Asthma Control Test (ACT) scores. Notably, poor indoor air quality was also linked to increased emergency department visits and reduced physical and mental HRQoL, highlighting not only symptom burden, but also healthcare consequences (100). Collectively, these findings provide compelling evidence that indoor air pollution plays a pivotal role in both the development of asthma and the worsening of disease control.
While the aforementioned studies focused on indoor environments, it is also important to consider that early-life exposure to both indoor and ambient air pollution may shape asthma susceptibility across the lifespan. In a large cohort study by Zanobetti et al (89) using data from the ECHO CREW Consortium, early-life exposure to PM2.5 and NO2 was shown to be associated with a significantly increased risk of childhood asthma by both ages 4 and 11. Notably, the risk was higher among children of African descent and those residing in socioeconomically disadvantaged communities, suggesting that environmental injustice amplifies asthma risk (89).
Of particular relevance is a population-based study conducted in Almaty, Kazakhstan, where researchers measured indoor air quality during the cold season. a period when households rely heavily on coal and other solid fuels for heating (101). The findings of that revealed alarmingly high concentrations of indoor PM2.5 that often markedly exceeded WHO safety limits. Even in indoor settings, such as homes and kindergartens, PM2.5 levels were found to reach levels associated with significant respiratory risk (101). These results underscore the acute need for policy-level interventions to mitigate indoor pollution and protect vulnerable populations, particularly children and individuals with chronic respiratory diseases such as asthma.
The implications for asthma management are profound. Prolonged exposure to indoor air pollutants can not only trigger and exacerbate asthma attacks, but can also contribute to a long-term decline in lung function, poor medication responsiveness and increased psychological stress, further decreasing HRQoL. This is particularly critical in LMICs, where healthcare access may be limited and asthma remains underdiagnosed and undertreated.
Given this context, indoor air pollution must be recognized as a top-tier public health priority in asthma prevention and management. Mitigation strategies may include promoting clean energy transitions, improving household ventilation, phasing out coal and biomass fuels, setting indoor air quality standards and expanding environmental monitoring programs. Public awareness campaigns about indoor air quality and its link to respiratory health should also be integrated into national health promotion initiatives. The control of indoor air pollution, particularly during high-risk periods such as the cold season represents a critical opportunity to reduce asthma burden and improve QoL in the urban areas of developing countries.
Allergen exposure is another key environmental factor affecting asthma severity and QoL (Table II). Common allergens such as dust mites, pollen, mold spores, pet dander and cockroach allergens can trigger airway inflammation and lead to increased symptom burden, particularly in individuals with allergic asthma (102,103). Seasonal variations in pollen levels, particularly in spring and the fall, often result in worsened symptoms and a greater reliance on medications (104,105). The presence of mold in damp indoor environments further contributes to poor respiratory health, particularly in humid climates or inadequately ventilated homes. Poor indoor air quality, combined with exposure to dust, household chemicals and second-hand smoke, increases the risk of uncontrolled asthma. Implementing allergen avoidance strategies, such as using high-efficiency particulate air (HEPA) filters, maintaining low indoor humidity, regular cleaning and limiting exposure to known allergens, can help improve asthma control (106,107). Additionally, immunotherapy for allergen desensitization may be beneficial for patients with severe allergic asthma.
Climate variability and extreme weather conditions further exacerbate asthma symptoms and contribute to fluctuations in disease severity (108-110). Hot and humid conditions promote higher concentrations of airborne allergens and mold growth, leading to increased respiratory distress in susceptible individuals. Conversely, cold air functions as a broncho-constrictor, triggering airway narrowing and worsening asthma attacks, particularly during the winter months (108-110).
Climate change has also led to longer and more intense pollen seasons, increasing allergic sensitization and exacerbations in patients with asthma (111). Additionally, wildfires and desert dust storms, which have become more frequent in a number of regions, significantly degrade air quality, exposing individuals to PM2.5 that can aggravate lung inflammation (112). To mitigate the impact of climate variability on asthma, public health initiatives should focus on early warning systems for air pollution spikes, improved respiratory health monitoring and climate-adaptive strategies, such as enhanced urban greenery and sustainable building designs to reduce indoor pollutant exposure (36,113).
Occupational exposure to irritants, such as chemicals, fumes and dust is a key environmental factor that affects patients with asthma, particularly those working in high-risk industries such as construction, agriculture, manufacturing and cleaning services (114,115). Prolonged exposure to workplace pollutants, such as asbestos, silica, pesticides and industrial gases increases the likelihood of developing occupational asthma (OA) and aggravates pre-existing respiratory conditions (14,116). Workers with OA often experience reduced lung function, higher absenteeism rates and impaired productivity, leading to a lower overall QoL. Addressing OA requires comprehensive workplace interventions, including improved ventilation systems, the use of personal protective equipment, strict adherence to occupational health and safety regulations, and early screening programs for workers in high-risk industries.
Among the various subtypes of asthma, OA and work-exacerbated asthma (WEA) represent a substantial yet often under-recognized proportion of adult asthma cases (117,118). Epidemiological studies estimate that up to 15-20% of adult asthma cases are directly attributable to occupational exposures, with an even higher proportion (25-30%) experiencing work-aggravated symptoms due to environmental irritants or allergens in the workplace (119). These conditions, although distinct in etiology, have a profound impact on the HRQoL of patients and impose significant socioeconomic burdens.
Patients with OA and WEA frequently encounter reduced lung function, poor asthma control, increased medication use and more frequent exacerbations compared to non-OA cases (120,121). Notably, both general HRQoL and asthma-specific HRQoL are markedly diminished in this group.
The study conducted by Alpaydin et al (122) found a significant positive association between asthma control, measured using the ACT, and QoL assessed through the Asthma Quality of Life Questionnaire (AQLQ). Specifically, each 1-point increase in the ACT score corresponds to a 0.129-point improvement in AQLQ scores. However, the agreement between ACT scores and guideline-based asthma control assessments was only moderate. The study also examined treatment adjustments based on ACT scores, noting that step-up therapy improved ACT scores in uncontrolled patients, but did not significantly enhance AQLQ scores, while step-down therapy in controlled patients did not negatively affect either measure (122). These findings suggest that while ACT is useful for monitoring asthma control, it may not fully capture QoL outcomes, underscoring the importance of complementary tools such as AQLQ for patients.
Another study examined work-related asthma (WRA) among 217 asthma patients in Ulsan, Korea, identifying a prevalence of 17%, with WEA accounting for 50% of WRA cases (119). WEA was associated with more severe asthma symptoms, including a higher number of outpatient visits, increased oral corticosteroid use, and lower asthma control test scores compared to OA and non-WRA. Despite its severity, patients with WEA had a lower rate of job changes than patients with OA (119). These findings highlight the impact of workplace exposure on asthma severity and the need for the improved recognition and management of WEA.
One of the defining challenges in the management of OA and WEA is the need for workplace modification or, in a number of cases, complete job changes, particularly when exposure to the causal agent cannot be eliminated. This has marked implications for income security, career trajectory and psychosocial well-being. Patients may face unemployment, underemployment, or forced career transitions, often with inadequate social support or compensation mechanisms, particularly in low- and middle-income countries. The colossal economic and social costs associated with job changes both to the individual and the health system, contribute to delayed diagnosis, underreporting and poor adherence to management guidelines.
Moreover, studies have shown that the delayed removal from exposure is associated with persistent airway inflammation, the incomplete recovery of lung function, and an irreversible decline in HRQoL (123-125). Early detection and intervention are, therefore, crucial. Despite this, OA remains underdiagnosed in a number of healthcare settings, partly due to the lack of routine occupational history taking and insufficient awareness among both clinicians and patients.
OA and WEA need to be recognized as a priority within public health and occupational safety frameworks, particularly due to their profound and lasting impact on HRQoL and socioeconomic outcomes. Policy-level actions are required to strengthen occupational health surveillance, ensure early recognition, and provide structured pathways for job retraining, financial support and rehabilitation. Addressing these factors will be key to improving long-term outcomes and reducing the burden of asthma in the working population.
Socioeconomic disparities further exacerbate the impact of environmental factors on asthma outcomes. Individuals from lower-income communities are more likely to reside in areas with high pollution levels, substandard housing and inadequate access to healthcare services (126). Limited financial resources often prevent patients with asthma from accessing appropriate medications, maintaining regular medical check-ups, or modifying their living environments to reduce exposure to triggers. Additionally, poor housing conditions, including overcrowding, dampness and exposure to pests, contribute to a greater incidence of uncontrolled asthma. Socioeconomic barriers also limit access to specialized asthma care, leading to higher hospitalization rates and poorer disease management (Fig. 1). Addressing these disparities requires policy-driven efforts to improve housing conditions, expand healthcare access, subsidize essential asthma medications and implement community-based asthma education programs.
Robust epidemiological evidence has demonstrated a clear dose-response association between PM2.5 concentrations and asthma-related health risks (127). Even modest, short-term increases in PM2.5 levels have been linked to significant increases in asthma exacerbations, emergency department visits and hospitalizations (128). According to the WHO, the recommended annual mean PM2.5 level should not be >5 µg/m³, and daily exposure should remain <15 µg/m³ (129). However, these thresholds are routinely exceeded in numerous developing and rapidly urbanizing regions, particularly during winter seasons when reliance on solid fuels for heating increases or during periods of intense traffic and industrial emissions. In some cities, PM2.5 levels have been reported to be 3- to 5-fold higher than the recommended limits, exposing large populations to respiratory risks (130,131).
One notable example is Almaty, Kazakhstan, where a recent population-based study revealed alarmingly high concentrations of indoor PM2.5 during the cold season (101). Measurements taken in homes, schools and kindergartens frequently exceeded WHO safety thresholds by up to 10-fold, reaching levels >150 µg/m³ (101). These concentrations are categorized as hazardous and are associated with significant respiratory damage, particularly among children and individuals with pre-existing respiratory conditions, such as asthma. These findings underscore the critical importance of public health action, particularly in addressing household heating practices, improving ventilation and transitioning toward cleaner energy sources.
The risks posed by air pollution are further compounded by the increasing effects of climate change. Rising global temperatures, shifting precipitation patterns and an increased frequency of extreme weather events such as heatwaves, cold spells, wildfires and dust storms all contribute to the worsening of asthma symptoms and overall disease burden (132). Warmer temperatures and elevated carbon dioxide levels have been shown to be associated with longer pollen seasons and heightened allergenicity of airborne particles, increasing the prevalence and severity of allergic asthma (133). Wildfires, which are becoming more frequent and severe due to prolonged droughts and land degradation, produce large quantities of PM2.5 and O3 precursors, which can deteriorate air quality over vast regions (134,135). Simultaneously, extreme cold weather events drive up indoor pollution by increasing dependence on biomass and coal fuels for heating, while flooding events can promote mold growth in homes, yet another potent asthma trigger (134,135).
These intersecting environmental pressures particularly affect vulnerable and low-income populations, who often reside in poorly insulated homes, lack access to clean energy and have limited capacity to respond or adapt to environmental hazards. Consequently, the burden of asthma disproportionately falls on those least equipped to manage its environmental determinants, further widening existing health inequities.
Addressing these interconnected challenges requires the implementation of integrated and forward-thinking adaptation strategies. Urban green infrastructure, including expanded tree canopies, vegetative buffers and accessible parks, can mitigate the urban heat island effect, reduce airborne pollutants and improve the overall air quality of densely populated areas (136). When carefully planned to avoid high-allergen species, green urban design can provide long-term respiratory health benefits. Likewise, promoting sustainable building designs that emphasize energy efficiency, clean heating technologies and improved indoor ventilation can greatly reduce household exposure to pollutants. These architectural and planning interventions need to be coupled with real-time air quality monitoring systems and public health alert mechanisms to allow individuals with asthma to minimize exposure during pollution peaks (137). Incorporating such systems into broader health surveillance frameworks will be critical in supporting early response and preventing acute health crises.
Equally important is the integration of climate-resilient thinking into healthcare planning. This includes ensuring reliable access to asthma medications during environmental emergencies, strengthening healthcare infrastructure to remain functional during extreme weather events, and training healthcare providers to recognize and address environmentally driven asthma symptoms. Public health education campaigns must also raise awareness of both indoor and outdoor air quality risks, and emphasize practical strategies for reducing exposure, particularly in high-risk groups.
Ultimately, air pollution and climate change should be recognized not as peripheral challenges, but as central, modifiable determinants of asthma morbidity and impaired QoL. The mounting evidence clearly demonstrates that exceeding PM2.5 thresholds is directly associated with worsened asthma outcomes and that environmental exposures, particularly when coupled with socioeconomic disadvantage, can accelerate the progression of disease and hinder asthma control. Failure to act on these insights will perpetuate avoidable health burdens and undermine long-term asthma management efforts. Thus, a systems-based, multi-sectoral approach, bridging environmental policy, urban planning, clinical care and social equity is essential to reduce the environmental drivers of asthma and to safeguard respiratory health in the face of a changing climate.
5. Healthcare accessibility
Healthcare accessibility is a fundamental determinant of the QoL of patients with bronchial asthma. Despite advancements in asthma treatment, disparities in healthcare access continue to hinder effective disease management, leading to increased hospitalizations, exacerbations and reduced overall well-being. The limited availability of specialized care, geographic disparities, socioeconomic barriers, medication affordability and insufficient patient education all contribute to poor asthma control and a decreased QoL (Fig. 1). Addressing these challenges is essential for ensuring that all patients receive timely, effective and equitable asthma care.
One of the most significant barriers to healthcare accessibility is the unequal distribution of medical resources, particularly between urban and rural areas (138,139). Patients residing in major cities generally have better access to pulmonologists, allergists and advanced diagnostic facilities, whereas those in rural and remote regions often rely on primary care physicians who may lack specialized training in asthma management (140). Studies have shown that patients with asthma residing in rural patients face higher rates of misdiagnosis, delayed treatment, and inadequate disease control, leading to more frequent exacerbations and hospitalizations (141,142). The lack of specialized care also limits access to advanced therapies, such as biologics, which are crucial for severe asthma cases. Expanding telemedicine services, training primary care physicians in asthma management and improving healthcare infrastructure in underserved areas can help bridge this gap and enhance asthma care for rural populations.
Socioeconomic barriers further impact healthcare accessibility and the ability of asthma patients to manage their condition effectively. A number of individuals with asthma, particularly those from low-income backgrounds, struggle to afford essential medications, diagnostic tests and follow-up appointments. ICS and long-acting bronchodilators, which are the cornerstone of asthma management, remain cost-prohibitive for numerous patients, leading to poor adherence and increased symptom severity (143,144). Additionally, individuals without health insurance or those with limited coverage often face difficulties obtaining specialist consultations, further delaying optimal disease management. The financial burden of asthma extends beyond medication costs, as frequent hospital visits, lost workdays and productivity loss also negatively affect the economic stability and QoL of patients. Implementing policies that subsidize essential asthma medications, as well as expanding insurance coverage and offering financial assistance programs can significantly improve medication adherence and disease outcomes.
The availability of emergency and primary healthcare services is another critical factor influencing asthma-related QoL. Patients with poorly controlled asthma often rely on emergency departments for acute exacerbations, which not only increases healthcare costs, but also reflects inadequate preventive care and disease monitoring (145,146). Frequent emergency visits are associated with increased psychological distress, lower functional capacity and an overall poorer QoL. Enhancing access to primary healthcare providers who can offer routine monitoring, personalized asthma action plans and early intervention strategies is crucial for reducing emergency hospitalizations and promoting long-term disease control (147). Encouraging the use of community-based asthma programs and integrating case management services into primary care settings can also provide patients with continuous support and disease education (148,149).
Medication accessibility and adherence play a fundamental role in determining asthma outcomes and QoL (150). Numerous patients do not adhere to their prescribed treatment regimens due to a lack of understanding about their condition, the fear of side-effects, or misconceptions about medication dependence (151). Poor adherence leads to uncontrolled symptoms, frequent exacerbations and an increased risk of hospitalization (152). Studies have shown that patient education programs focusing on correct inhaler techniques, the importance of controller medications, and trigger avoidance significantly improve adherence and disease management (150,153,154). Pharmacists and healthcare providers need to play a more active role in educating patients and ensuring that they receive affordable, high-quality medications tailored to their disease severity (155). Expanding access to generic asthma medications and improving patient awareness of inhaler use can lead to increased adherence rates and improved QoL.
Language barriers and health literacy also contribute to disparities in asthma care. Patients with limited health literacy may struggle to understand prescription instructions, symptom monitoring guidelines and emergency action plans, resulting in inadequate disease management (156,157). Non-native speakers may also face difficulties in communicating with healthcare providers, leading to misinterpretations of medical advice and improper medication use. Implementing multilingual asthma education programs, culturally tailored healthcare services, and visual-based instructional materials can help overcome these barriers and empower patients to take a more active role in managing their condition.
Psychosocial support and mental health care are often overlooked aspects of healthcare accessibility that significantly affect the QoL of patients with asthma (158,159). Living with a chronic respiratory condition can lead to increased stress, anxiety and depression, which in turn can exacerbate asthma symptoms. Limited access to mental health services means that many patients do not receive adequate psychological support, further worsening their overall well-being (160). Integrating mental health screenings into routine asthma care, offering counselling services, and incorporating stress-management techniques into treatment plans can help improve both physical and emotional health outcomes.
Improving healthcare accessibility requires a multifaceted approach that includes expanding healthcare infrastructure, reducing financial barriers, enhancing patient education and integrating technology into asthma management. In this context, telemedicine has emerged as a valuable tool in bridging healthcare gaps, allowing patients to consult with specialists remotely and receive real-time guidance on symptom management (161,162). Mobile health applications and wearable devices that monitor peak flow rates, medication adherence, and air quality levels can further enhance patient engagement and early intervention strategies (163,164).
In the recent study by Suvarna et al (165) the effectiveness of telemedicine was directly compared to traditional in-person follow-up in children with asthma aged 7-17 years. Their non-inferiority trial demonstrated that telemedicine follow-up achieved similar improvements in asthma control (measured by ACT/C-ACT scores) and Pediatric Quality of Life Index (PQLI) scores over a 3-month period. The differences between telemedicine and in-person visits were not statistically significant (mean ACT/C-ACT difference: -0.35, P=0.09; PQLI difference: P=0.91), suggesting that telemedicine may serve as a viable and effective alternative to in-person consultations. Importantly, parent satisfaction was high (mean satisfaction score: 3.8/5), further supporting the acceptability of remote asthma care, particularly in remote or resource-constrained settings, and during pandemic scenarios where in-person care may be limited (165).
Complementing these findings, Alcoceba-Herrero et al (166) evaluated a more technology-integrated approach through a novel clinical decision support system (CDSS) enabled by remote patient monitoring and wearable devices. Although that study primarily focused on patients with COVID-19, it identified asthma as a significant predictor of severe alerts (odds ratio, 1.74; P=0.002), underscoring the vulnerability of this population and the critical need for real-time surveillance. The system generated significantly more alerts (>61,000 vs. 1,800 in the control group), but the use of artificial intelligence (AI) ensured that this did not overwhelm healthcare providers (133). These results highlight the potential of telemonitoring to proactively detect deterioration in chronic disease patients, such as those with asthma, and tailor timely interventions without increasing clinical workload. The incorporation of AI-driven alert systems may become an integral component of asthma management in the near future.
Further expanding on the benefits of digital health, the randomized clinical trial by Cabrerizo-Carreño et al (167) assessed the long-term impact (over a period of 52 weeks) of the ESTOI mobile health application among patients with asthma in Spain (167). The intervention group received a comprehensive, personalized care approach through the application, which included symptom tracking, treatment plans, educational materials and direct communication with a medical team. That study aimed to evaluate asthma control (ACT scores), treatment adherence (TAI) and patient-reported QoL (AQLQ), along with clinical parameters, such as spirometry and biomarkers. Though detailed results are pending in the abstract, the study underscores the utility of mobile apps in facilitating personalized, continuous asthma care, and enhancing self-management and patient engagement over time (167).
Based on the comprehensive discussion of healthcare accessibility in asthma care, feasibility analyses for policy recommendations, particularly those aimed at expanding insurance coverage and subsidizing essential asthma treatments are both timely and necessary. The currently available evidence illustrates that barriers to access, including the affordability of medications, uneven geographic distribution of specialized services, and lack of health literacy support, are not merely logistical challenges, but are directly linked to poorer clinical outcomes and a diminished QoL of patients with asthma.
From a policy standpoint, expanding insurance coverage to include essential asthma medications (such as ICS and long-acting bronchodilators) and specialist services would likely yield a favorable cost-benefit profile. Multiple studies have shown that poor asthma control results in higher rates of emergency department visits, hospitalizations, absenteeism and lost productivity (23,168,169). These indirect costs, when added to the direct medical expenses of acute care, often far exceed the cost of preventive and maintenance therapies. Therefore, policies that reduce out-of-pocket costs for controller medications and diagnostic services could prevent exacerbations and reduce healthcare utilization, particularly among low-income and uninsured populations. Moreover, investing in early access to biologics and specialist consultation for patients with severe asthma can prevent long-term deterioration, irreversible lung function decline, and the accumulation of healthcare costs due to repeated acute care episodes.
Economic models from various healthcare systems support the notion that preventive, community-based asthma care is cost-effective or even cost-saving over the long term. For example, evidence from US-based Medicaid populations has shown that every dollar spent on asthma education and case management can save up to $7 in reduced emergency care and hospitalization costs (170,171). Similarly, countries with universal or subsidized coverage for asthma therapies such as Finland and Canada report significantly better population-level asthma control and QoL, reinforcing the feasibility of broad insurance coverage as a scalable policy strategy (172-176).
Telemedicine and digital health technologies provide additional pathways to expand healthcare access, while containing costs. A number of studies have demonstrated that remote consultations, AI-assisted monitoring, and mobile apps for asthma management were clinically non-inferior to in-person care and associated with high user satisfaction (177,178). Of note, such platforms eliminate geographic barriers, reduce transportation and time costs, and enable proactive intervention before clinical deterioration occurs. The scalability and relative affordability of these interventions suggest strong feasibility for public health systems, particularly in settings with limited access to specialists. Including these services in insurance benefit packages, whether public or private, can ensure that digital tools are accessible, not only to tech-savvy or affluent users, but to the broader population of patients with asthma.
A key element in feasibility analysis is health equity. Without financial protection, patients in lower-income brackets may continue to underuse necessary medications, delay care, or rely solely on emergency services all of which deepen health disparities. Expanding insurance coverage, coupled with patient subsidies and community outreach programs, can act as powerful equalizers. Notably, such measures need to be accompanied by education programs and culturally appropriate care models to ensure effective use of services once access is granted.
Governments and healthcare organizations must work together to ensure equitable access to quality asthma care by implementing policies that support universal healthcare coverage, subsidized medications and community-based asthma programs (142).
6. Psychological factors
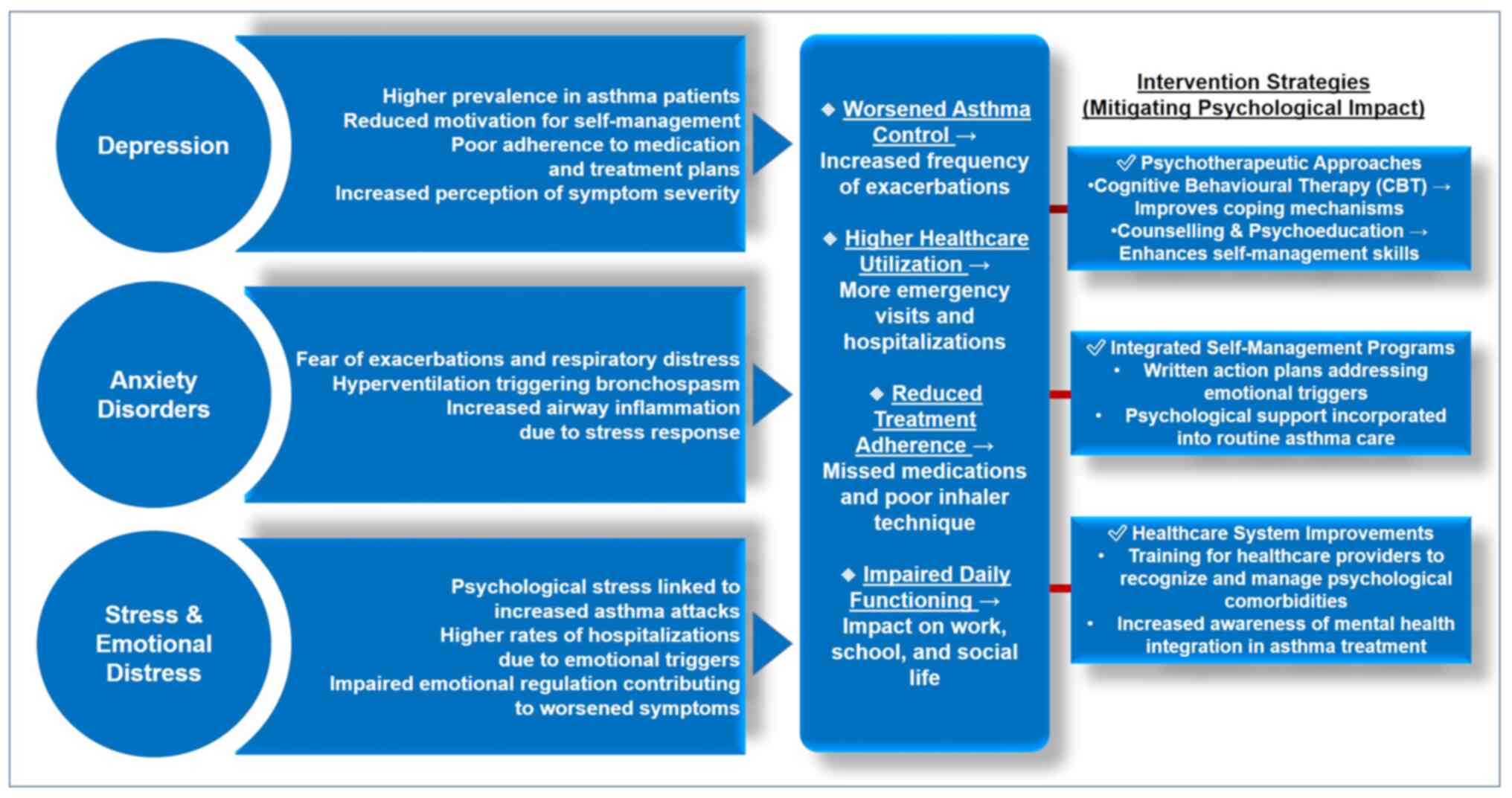
Psychological factors play a critical role in the management and QoL of patients with bronchial asthma. The interplay between asthma and psychological conditions, such as anxiety and depression, can create a complex cycle that exacerbates both respiratory symptoms and mental health issues (179,180). Understanding these dynamics is crucial for developing comprehensive treatment strategies that address the psychological aspects of asthma management.
Research indicates that patients with asthma experience a greater prevalence of psychological comorbidities compared to the general population (181,182). A previous review of various studies demonstrated that anxiety disorders are particularly common among asthmatic patients, with estimates suggesting that ~50% of individuals with asthma also suffer from anxiety (183). This association is often bidirectional; while asthma can lead to increased anxiety due to the fear of exacerbations and respiratory distress, anxiety can also worsen asthma control by triggering physiological responses that lead to bronchospasm and airway inflammation.
Depression is another prevalent psychological condition among patients with asthma (Fig. 2). Previous studies have indicated that depressive disorders are significantly more common in individuals with asthma than in those without the condition (184,185). The impact of psychological factors extends beyond individual symptoms; it influences overall disease management and patient outcomes. Patients with asthma who experience high levels of stress or negative emotions are more likely to report severe symptoms and experience more frequent exacerbations. Emotional distress has been associated with an increased risk of asthma attacks, suggesting that effective emotional regulation may contribute to better asthma control (159,186-188).
Psychotherapeutic interventions have shown promise in addressing the psychological needs of asthmatic patients (189). Various approaches, including cognitive behavioral therapy (CBT), counselling and psycho-educational interventions, have been studied for their effectiveness in improving both psychological well-being and asthma management. For instance, CBT has been found to help patients develop coping strategies for managing their condition, leading to reductions in anxiety levels and improvements in self-management skills (190).
Additionally, self-management programs that incorporate psychological support have proven beneficial for asthmatic patients. These programs often include written action plans that guide patients on how to manage their symptoms effectively while also addressing emotional aspects related to their condition. Studies have indicated that when psychological support is integrated into standard asthma care, patients experience an improved QoL, greater adherence to treatment protocols and reduced rates of exacerbations (191,192).
Despite the clear link between psychological factors and asthma management, there remains a significant gap in the recognition and treatment of these issues within the healthcare system. A number of healthcare providers may not be adequately trained to identify or address the psychological needs of their asthmatic patients. This oversight can result in missed opportunities for intervention and support.
The interplay between bronchial asthma and mental health conditions, such as anxiety and depression is bidirectional and self-perpetuating, contributing to worsened symptom perception, reduced treatment adherence and increased morbidity. A mechanistic understanding of this association is critical for designing comprehensive asthma management strategies that integrate mental health support alongside physical treatment.
The biological underpinnings of the asthma-psychology association are rooted in stress physiology, particularly activation of the hypothalamic-pituitary-adrenal (HPA) axis and the autonomic nervous system (193). Psychological stress, anxiety and depression can activate the HPA axis, resulting in the release of cortisol and catecholamines (194). These hormonal shifts influence immune function and increase airway inflammation and hyper-reactivity, thereby exacerbating asthma symptoms (195). Concurrently, heightened vagal tone and parasympathetic over-activation can directly trigger bronchoconstriction, leading to acute dyspnea and wheezing (196,197). These physiological responses reinforce the psychological distress experienced by patients, thus creating a feedback loop in which psychological and respiratory symptoms amplify one another (196,197).
This cycle is supported by population data demonstrating significantly higher prevalence rates of anxiety and depression in patients with asthma compared to the general population. In fact, a growing body of research highlights that individuals with asthma are at a significantly increased risk of developing psychiatric comorbidities, particularly anxiety and depression, compared to the general population (183,198). These mental health issues not only coexist with asthma, but may also worsen disease outcomes by affecting self-management, medication adherence and overall QoL.
In a real-world clinical study by Beyhan Sagmen et al (199), involving 88 adult patients with asthma, the prevalence of anxiety was found to be 55% and depression 62%, far exceeding general population estimates. Their findings also revealed that these psychological symptoms were associated with poorer asthma control, as evidenced by significantly lower ACT scores among affected patients. Females were disproportionately affected, with 61% reporting anxiety compared to 32% of males (P=0.023). That study underscored the importance of integrating mental health screening into routine asthma care and highlights the role of coping strategies in mediating these associations (199).
Further expanding on the mechanistic links, in another study, Caulfield (183) provided a psycho-neuro-immunological perspective by emphasizing that individuals with asthma are up to 3-fold more likely to develop internalizing disorders, namely anxiety and depression, compared to non-asthmatic individuals. This heightened risk is considered to be driven in part by chronic systemic inflammation and environmental exposures such as air pollution, which contribute to both airway inflammation and neuro-inflammation. The aforementioned review outlined how asthma is not merely a respiratory disease, but a systemic condition with broad psychological implications, especially during developmental stages, and calls for integrated treatments that target both inflammation and mental health symptoms (183).
Similarly, Stubbs et al (200) examined 140 patients with severe asthma and found that 47% of the patients exhibited symptoms of anxiety and/or depression, with 13% of patients reporting both symptoms. These individuals had a significantly poorer asthma control and QoL compared to those without psychiatric symptoms. Moreover, their multivariate analysis identified dysfunctional breathing, dyspnea and obesity as key clinical predictors of psychological comorbidities in this population (200). Their study reinforces the need for a multidimensional approach to asthma care, where psychological health is recognized as a critical component of disease severity and management (200).
Taken together, these studies make a compelling case for routine screening of anxiety and depression in asthma care, particularly in patients with poor asthma control, frequent exacerbations, or severe disease. They also point to the need for integrated care pathways, including mental health support, pulmonary rehabilitation and behavioral interventions, to improve long-term outcomes in this vulnerable population.
The findings of a previous meta-analytic estimated that up to 50% of individuals with asthma also meet diagnostic criteria for anxiety disorders, while the rates of depressive symptoms were 1.5-2-fold higher than in non-asthmatic controls (188). Emotional distress has been temporally linked to acute asthma exacerbations and is associated with increased healthcare utilization and poor disease control. Furthermore, studies indicate that subjective symptom burden is often more severe in patients with psychological comorbidities, even when objective lung function remains stable, highlighting the influence of cognitive-emotional processes on disease perception (201,202).
Notably, psychological interventions, particularly CBT has demonstrated significant efficacy in improving both mental health and asthma-related outcomes (203). CBT helps patients reframe catastrophic thinking, manage panic related to dyspnea, and develop structured coping strategies, which can lead to reductions in anxiety and depression as well as improved self-efficacy in asthma self-management (159).
Randomized controlled trials have reinforced these findings (159,189,204). Despite this strong evidence base, psychological comorbidities remain under-recognized and undertreated in clinical asthma care. A number of healthcare professionals lack training in assessing mental health conditions, and psychological screening is rarely part of routine asthma evaluations. This gap presents a missed opportunity to deliver holistic, patient-centered care that addresses the full spectrum of asthma burden. Implementing brief mental health screenings, such as the GAD-7 or PHQ-9, in asthma clinics can facilitate early identification and timely referral to psychological services (205,206).
To summarize, the psychological factors, such as anxiety and depression significantly affect the QoL of patients with bronchial asthma. Addressing these issues through integrated care approaches, combining pharmacological treatments with psychotherapeutic interventions can lead to improved patient outcomes. By prioritizing mental health alongside physical health in asthma management strategies, healthcare providers can enhance the overall well-being of individuals living with this chronic condition. Comprehensive training for healthcare professionals on recognizing and treating psychological comorbidities will be essential for fostering a more holistic approach to asthma care.
7. Study limitations
Despite providing a comprehensive synthesis of the existing literature, the present review has several limitations that should be acknowledged. First and foremost, selection bias may have influenced the findings. The present review does not clearly describe the methodology used for study selection, including inclusion and exclusion criteria, search strategy, or the number of databases consulted. As a result, there is a risk that relevant studies may have been unintentionally omitted or that studies with positive findings were preferentially included, leading to a skewed representation of the evidence.
Furthermore, the review lacks a systematic approach in evaluating the quality of the included studies. Without formal quality assessment or critical appraisal tools (e.g., PRISMA, GRADE), it is difficult to determine the strength of the evidence supporting each factor affecting the quality of life in cancer patients.
Another limitation is the heterogeneity of the included studies. The review combines findings from diverse populations, cancer types, treatment modalities and geographic regions without clearly addressing how these differences may affect the generalizability of the results. Cultural, socioeconomic and healthcare system-related differences may significantly influence patients' quality of life, yet these contextual factors are not sufficiently analyzed or controlled for.
Additionally, the review largely relies on qualitative summarization rather than quantitative synthesis or meta-analysis, which limits the ability to determine the magnitude of effect for each factor discussed. This narrative approach also introduces potential interpretation bias, as the synthesis is based on the authors' subjective interpretation of study findings.
8. Conclusion
The QoL of individuals living with bronchial asthma is shaped by a dynamic interplay of socio-demographic, clinical, environmental, psychological and healthcare-related factors. Disparities in education, sex, income and place of residence, particularly between urban and rural communities, significantly affects the ability of patients to access care, adhere to treatment and achieve optimal disease control. Clinical determinants, such as asthma severity, comorbidities and medication adherence are closely linked to symptom burden and the risk of exacerbations. Moreover, environmental exposures, including air pollution, allergen load and climate variability, continue to be major external drivers of poor asthma outcomes, especially in areas with weak environmental regulation or reliance on polluting fuels.
Healthcare accessibility remains a major barrier, particularly in low-resource countries, particularly in Central Asia. In Kazakhstan, for example, stark urban-rural disparities regarding access to pulmonologists, diagnostic services and essential medications limit the reach and effectiveness of asthma care. Addressing these gaps is essential for reducing asthma-related morbidity and improving QoL. Moreover, psychological comorbidities, such as anxiety and depression are highly prevalent among asthma patients and often go undiagnosed and untreated, compounding the disease burden.
To meaningfully address these challenges, a comprehensive and multi-sectoral approach is required. Improving asthma outcomes requires more than medical intervention, it demands coordinated action across healthcare, environmental and social policy domains. Health ministries need to work in tandem with environmental agencies, urban planners and civil society organizations to develop integrated strategies that address both medical and environmental determinants of asthma. This includes enforcing clean air policies, promoting access to clean household energy, expanding asthma education programs, and integrating mental health services into routine asthma care. NGOs and community organizations can also play a vital role in delivering culturally appropriate education, facilitating access to services, and advocating for marginalized groups.
The tailored strategies need to focus on strengthening rural health infrastructure, supporting primary care providers with asthma-specific training and leveraging telemedicine to bridge geographic gaps. Investment in national asthma registries, environmental health monitoring and patient-centered data systems will also be crucial for evidence-based planning and evaluation.
Ultimately, the successful management of asthma and the improvement of the QoL of patients require an approach that transcends clinical boundaries. Through cross-sector collaboration, policy alignment and investment in equitable, preventive care, low- and middle-income countries in Central Asia can lead the way in creating sustainable, inclusive asthma care systems that respond to the unique needs of their populations.
Acknowledgements
The authors would like to thank the S.D. Asfendiyarov Kazakh National Medical University (Almaty, Kazakhstan) for the administrative and technical support provided.
Funding
Funding: No funding was received.
Availability of data and materials
Not applicable.
Authors' contributions
MM was involved in the writing of the original draft of the manuscript, in the reviewing and editing of the manuscript, and in project administration. NA was involved in the editing of the manuscript and in the cconceptualization of the study. AD was involved in the writing of the manuscript. DB was involved in the conceptualization of the study. AT was involved in the analysis of the literature analysis and in acquisition of data from the literature. AO was involved in the collection of data from the literature, as well as in the conceptualization of the study. BA was involved in the conceptualization of the study. TS was involved in the writing of the original draft, in the review and editing of the manuscript, and in study supervision. All the authors have read and approved the final version of the manuscript and agreed to be accountable for all aspects of the work. Data authentication is not applicable.
Ethics approval and consent to participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
|
Garg R, Piplani M, Singh Y, Bhateja P and Rana R: An overview of integrated risk factors with prevention and prevalence of asthma at the global level. Curr Tradit Med. 10:71–81. 2024. | |
|
Kharusi ZA, Kalbani RA and Al-Hadhrami R: Frequency of asthma exacerbations and upper respiratory tract infections among adults with asthma according to vaccination status. Sultan Qaboos Univ Med J. 24:70–75. 2024.PubMed/NCBI View Article : Google Scholar | |
|
Ora J, De Marco P, Gabriele M, Cazzola M and Rogliani P: Exercise-induced asthma: Managing respiratory issues in athletes. J Funct Morphol Kinesiol. 9(15)2024.PubMed/NCBI View Article : Google Scholar | |
|
Wu P, Hu Y and Yan X: Progress in research into the effectiveness of pulmonary rehabilitation in children with asthma-a narrative review. J Asthma Allergy. 17:743–750. 2024.PubMed/NCBI View Article : Google Scholar | |
|
Vinnikov D, Raushanova A, Mukatova I, Nurpeissov T, Кushekbayeva A, Toxarina A, Yessimova B, Bespayeva F and Brimkulov N: Asthma control in Kazakhstan: Need for urgent action. BMC Pulm Med. 23(7)2023.PubMed/NCBI View Article : Google Scholar | |
|
Agache I, Adcock IM, Akdis CA, Akdis M, Bentabol-Ramos G, van den Berge M, Boccabella C, Canonica WG, Caruso C, Couto M, et al: The bronchodilator and anti-inflammatory effect of long-acting muscarinic antagonists in asthma: An EAACI position paper. Allergy. 80:380–394. 2025.PubMed/NCBI View Article : Google Scholar | |
|
Seshadri N, Faig W, Young LR and Hill DA: Risk factors for hospitalization in subspecialty patients with severe persistent asthma. Respir Med. 235(107867)2024.PubMed/NCBI View Article : Google Scholar | |
|
Mortimer K, Reddel HK, Pitrez PM and Bateman ED: Asthma management in low and middle income countries: Case for change. Eur Respir J. 60(2103179)2022.PubMed/NCBI View Article : Google Scholar | |
|
Reddel HK, Bacharier LB, Bateman ED, Brightling CE, Brusselle GG, Buhl R, Cruz AA, Duijts L, Drazen JM, FitzGerald JM, et al: Global initiative for asthma strategy 2021. Executive summary and rationale for key changes. Arch Bronconeumol. 58:35–51. 2022.PubMed/NCBI View Article : Google Scholar | |
|
Levy ML, Bacharier LB, Bateman E, Boulet LP, Brightling C, Buhl R, Brusselle G, Cruz AA, Drazen JM, Duijts L, et al: Key recommendations for primary care from the 2022 global initiative for asthma (GINA) update. NPJ Prim Care Respir Med. 33(7)2023.PubMed/NCBI View Article : Google Scholar | |
|
Chakaya J and Aï-Khaled N: Global asthma report 2022: A wake-up call to enhance care and treatment for asthma globally. Int J Tuberc Lung Dis. 26:999–1000. 2022.PubMed/NCBI View Article : Google Scholar | |
|
Symvoulakis EK, Stachteas P, Smyrnakis E, Volkos P, Mantadaki AE, Karelis A, Petraki C, Nioti K, Mastronikolis S, Antoniou AM and Linardakis M: Multiple behavioral risk factors as assets for chronic disease prevention: Observations from urban primary care settings in Crete, Greece. Cureus. 16(e56711)2024.PubMed/NCBI View Article : Google Scholar | |
|
Omotola OJ, Tobore IO, Kolawole SJ, Olasimbo OA, Emmanuel LA, Temitope OO, Fikayo BE and Olufemi OA: Associated factors and disability burden among adolescent and adult nigerians with bronchial asthma. Ethiop J Health Dev. 38:1–7. 2024. | |
|
Walters GI, Reilly C, Le Moual N, Huntley CC, Hussein H, Marsh J, Bahron A, Krishna MT and Mansur AH: Asthma control in severe asthma and occupational exposures to inhalable asthmagens. BBMJ Open Respir Res. 11(e001943)2024.PubMed/NCBI View Article : Google Scholar | |
|
Lv JJ, Kong XM, Zhao Y, Li XY, Guo ZL, Zhang YJ and Cheng ZH: Global, regional and national epidemiology of allergic disorders in children from 1990 to 2019: Findings from the global burden of disease study 2019. BMJ Open. 14(e080612)2024.PubMed/NCBI View Article : Google Scholar | |
|
Boulet LP, Lavoie KL, Raherison-Semjen C, Kaplan A, Singh D and Jenkins CR: Addressing sex and gender to improve asthma management. NPJ Prim Care Respir Med. 32(56)2022.PubMed/NCBI View Article : Google Scholar | |
|
Chowdhury NU, Guntur VP, Newcomb DC and Wechsler ME: Sex and gender in asthma. Eur Respir Rev. 30(210067)2021.PubMed/NCBI View Article : Google Scholar | |
|
Averell CM, Laliberté F, Germain G, Duh MS, Rousculp MD, MacKnight SD and Slade DJ: Impact of adherence to treatment with inhaled corticosteroids/long-acting β-agonists on asthma outcomes in the United States. Ther Adv Respir Dis. 16(17534666221116997)2022.PubMed/NCBI View Article : Google Scholar | |
|
Suh DI and Johnston SL: The Wiser strategy of using beta-agonists in asthma: Mechanisms and rationales. Allergy Asthma Immunol Res. 16:217–234. 2024.PubMed/NCBI View Article : Google Scholar | |
|
Rasp E, Rönö K, But A, Gissler M, Härkki P, Heikinheimo O and Saavalainen L: Burden of somatic morbidity associated with a surgically verified diagnosis of endometriosis at a young age: A register-based follow-up cohort study in Finland. Hum Reprod. 40:623–632. 2025.PubMed/NCBI View Article : Google Scholar | |
|
Hansen S, von Bülow A, Sandin P, Ernstsson O, Janson C, Lehtimäki L, Kankaanranta H, Ulrik C, Aarli BB, Fues Wahl H, et al: Prevalence and management of severe asthma in the Nordic countries: Findings from the NORDSTAR cohort. ERJ Open Res. 9(00687)2023.PubMed/NCBI View Article : Google Scholar | |
|
Ye W, Xu X, Ding Y, Li X and Gu W: Trends in disease burden and risk factors of asthma from 1990 to 2019 in belt and road initiative countries: Evidence from the global burden of disease study 2019. Ann Med. 56(2399964)2024.PubMed/NCBI View Article : Google Scholar | |
|
Leso V, Candia C, Pacella D, Molino A, Nocera C, Maniscalco M and Iavicoli I: Quality of life and work functionality in severe asthma patients: The impact of biological therapies. J Occup Med Toxicol. 19(8)2024.PubMed/NCBI View Article : Google Scholar | |
|
Perelman NL and Kolosov VP: Differences in the health-related quality of life in patients with asthma living in urban and rural areas in the Amur region of russian federation. PLoS One. 18(e0284683)2023.PubMed/NCBI View Article : Google Scholar | |
|
Hsiao CC, Cheng CG, Hong ZT, Chen YH and Cheng CA: The influence of fine particulate matter and cold weather on emergency room interventions for childhood asthma. Life (Basel). 14(570)2024.PubMed/NCBI View Article : Google Scholar | |
|
Kerr GH, van Donkelaar A, Martin RV, Brauer M, Bukart K, Wozniak S, Goldberg DL and Anenberg SC: Increasing racial and ethnic disparities in ambient air pollution-attributable morbidity and mortality in the United States. Environ Health Perspect. 132(37002)2024.PubMed/NCBI View Article : Google Scholar | |
|
Górski P, Białas AJ and Piotrowski WJ: Aging lung: Molecular drivers and impact on respiratory diseases-a narrative clinical review. Antioxidants (Basel). 13(1480)2024.PubMed/NCBI View Article : Google Scholar | |
|
Armstrong S, Harris C, Kazemi M, Lunt A, Peacock J and Greenough A: Labor status at delivery and lung function in extremely prematurely born young adults. Pediatr Pulmonol. 60(e27440)2025.PubMed/NCBI View Article : Google Scholar | |
|
Koskela-Staples NC, Moorman EL, Jackson E, Fisher CL and Fedele DA: A systematic review of parent-child communication in pediatric asthma. J Pediatr Psychol. 50:205–232. 2025.PubMed/NCBI View Article : Google Scholar | |
|
Yeşilkaya S, Aksu K, Tuğçe Vural Solak G, Akkale O, Telli O, Tuğlu HC, Köycü Buhari G, Bahçecioğlu SN and Demir S: Variables predicting clinical remission among adults with severe asthma treated with biologic agents. Eur Ann Allergy Clin Immunol. 56:219–226. 2024.PubMed/NCBI View Article : Google Scholar | |
|
Harvey BJ and Mcelvaney NG: Sex differences in airway disease: Estrogen and airway surface liquid dynamics. Biol Sex Differ. 15(56)2024.PubMed/NCBI View Article : Google Scholar | |
|
Miligkos M, Oh J, Kwon R, Konstantinou GΝ, Kim S, Yon DK and Papadopoulos NG: Epidemiology of asthma across the ages. Ann Allergy Asthma Immunol. 134:376–384.e13. 2025.PubMed/NCBI View Article : Google Scholar | |
|
Anastasia P, Eleni T, Eleftheria M, Xenia N, Eygenia P, Kyriakos S, Katerina D, Petros B, Stelios L and Georgios H: Depression levels influence the rate of asthma exacerbations in females. J Pers Med. 11(586)2021.PubMed/NCBI View Article : Google Scholar | |
|
Yang-Huang J, van Grieken A, van Meel ER, He H, de Jongste JC, Duijts L and Raat H: Sociodemographic factors, current asthma and lung function in an urban child population. Eur J Clin Invest. 50(e13277)2020.PubMed/NCBI View Article : Google Scholar | |
|
Busby J, Price D, Al-Lehebi R, Bosnic-Anticevich S, van Boven JFM, Emmanuel B, FitzGerald JM, Gaga M, Hansen S, Hew M, et al: Impact of socioeconomic status on adult patients with asthma: A population-based cohort study from UK primary care. J Asthma Allergy. 14:1375–1388. 2021.PubMed/NCBI View Article : Google Scholar | |
|
Bush A, Byrnes CA, Chan KC, Chang AB, Ferreira JC, Holden KA, Lovinsky-Desir S, Redding G, Singh V, Sinha IP and Zar HJ: Social determinants of respiratory health from birth: Still of concern in the 21st century? Eur Respir Rev. 33(230222)2024.PubMed/NCBI View Article : Google Scholar | |
|
Vinnikov D, Raushanova A, Romanova Z and Tulekov Z: Health-related quality of life in a general population sample in Kazakhstan and its sociodemographic and occupational determinants. Health Qual Life Outcomes. 19(199)2021.PubMed/NCBI View Article : Google Scholar | |
|
Ghozali MT and Urrohmah UA: Determining the relationship between the knowledge on self-management and levels of asthma control among adult asthmatic patients: A cross-sectional study. J Med Life. 16:442–446. 2023.PubMed/NCBI View Article : Google Scholar | |
|
Alyas S, Hussain R, Ababneh BF, Ong SC and Babar ZU: Knowledge, perceptions, facilitators, and barriers towards asthma self-management among patients: A systematic review of the literature. Explor Res Clin Soc Pharm. 17(100558)2024.PubMed/NCBI View Article : Google Scholar | |
|
Radney A, Lee JY, Xu A, Steinke HR, Mengo C and Johnson-Motoyama M: Racial and ethnic disparities in healthcare utilization among children in U.S. foster care: Recommendations to challenge the status quo based on a scoping review. Child Youth Serv Rev. 162(107687)2024. | |
|
Lawson Y, Mpasi P, Young M, Comerford K and Mitchell E: A review of dairy food intake for improving health among black infants, toddlers, and young children in the US. J Natl Med Assoc. 116:228–240. 2024.PubMed/NCBI View Article : Google Scholar | |
|
Mseke EP, Jessup B and Barnett T: Impact of distance and/or travel time on healthcare service access in rural and remote areas: A scoping review. J Transp Health. 37(101819)2024. | |
|
Coombs NC, Campbell DG and Caringi J: A qualitative study of rural healthcare providers' views of social, cultural, and programmatic barriers to healthcare access. BMC Health Serv Res. 22(438)2022.PubMed/NCBI View Article : Google Scholar | |
|
Chowdhury J and Ravi RP: Healthcare accessibility in developing countries: A global healthcare challenge. J Clin Biomed Res. 4:1–5. 2022. | |
|
Ispayeva Z, Bekmagambetova R, Mustafina M, Kovzel E, Tusupbekova G, Morenko M, Saliev T, Tanabayeva S and Fakhradiyev I: Reliability and validity of the Kazakh-language act questionnaire as an asthma control tool. Georgian Med News. 6:85–90. 2024.PubMed/NCBI | |
|
Chung KF, Dixey P, Abubakar-Waziri H, Bhavsar P, Patel PH, Guo S and Ji Y: Characteristics, phenotypes, mechanisms and management of severe asthma. Chin Med J (Engl). 135:1141–1155. 2022.PubMed/NCBI View Article : Google Scholar | |
|
McDowell PJ, Busby J, Hanratty CE, Djukanovic R, Woodcock A, Walker S, Hardman TC, Arron JR, Choy DF, Bradding P, et al: Exacerbation profile and risk factors in a type-2-low enriched severe asthma cohort: A clinical trial to assess asthma exacerbation phenotypes. Am J Respir Crit Care Med. 206:545–553. 2022.PubMed/NCBI View Article : Google Scholar | |
|
Kun W, Xiaomei C, Lei Y and Huizhi Z: Modulating Th1/Th2 drift in asthma-related immune inflammation by enhancing bone mesenchymal stem cell homing through targeted inhibition of the Notch1/Jagged1 signaling pathway. Int Immunopharmacol. 130(111713)2024.PubMed/NCBI View Article : Google Scholar | |
|
Liu T, Woodruff PG and Zhou X: Advances in non-type 2 severe asthma: From molecular insights to novel treatment strategies. Eur Respir J. 64(2300826)2024.PubMed/NCBI View Article : Google Scholar | |
|
Mardi A, Abdolmohammadi-Vahid S, Sadeghi SA, Jafarzadeh S, Abbaspour-Aghdam S, Hazrati A, Mikaeili H, Valizadeh H, Sadeghi A, Ahmadi M and Nadiri M: Nanocurcumin modulates Th17 cell responses in moderate and severe COPD patients. Heliyon. 10(e30025)2024.PubMed/NCBI View Article : Google Scholar | |
|
Gohal G, Moni SS, Bakkari MA and Elmobark ME: A review on asthma and allergy: Current understanding on molecular perspectives. J Clin Med. 13(5775)2024.PubMed/NCBI View Article : Google Scholar | |
|
Krsmanović L, Arsović N, Bokonjić D, Nešić V, Dudvarski Z, Pavlović D, Dubravac Tanasković M, Ristić S, Elez-Burnjaković N, Balaban R, et al: The impact of cytokines on health-related quality of life in adolescents with allergic rhinitis. Biomedicines. 12(428)2024.PubMed/NCBI View Article : Google Scholar | |
|
Yatsuzuka K, Muto J, Shiraishi K, Fujisawa Y and Murakami M: Paradoxical eczema associated with interleukin-17A inhibitor use in a patient with generalized pustular psoriasis accompanied by asthma. Cureus. 16(e64680)2024.PubMed/NCBI View Article : Google Scholar | |
|
Pandey MK, Verma SK, Ahamad V and Kumari R: Circulating inflammatory mediators in COPD: A multimarker analysis of inflammatory biomarkers: Interleukin-6, -8, -10, and tumor necrosis factor-α alo with Leptin across disease stages. Indian J Respir Care. 13:34–42. 2024. | |
|
Sunata K, Miyata J, Kawashima Y, Konno R, Ishikawa M, Hasegawa Y, Onozato R, Otsu Y, Matsuyama E, Sasaki H, et al: Inflammatory profile of eosinophils in asthma-COPD overlap and eosinophilic COPD: a multi-omics study. Front Immunol. 15(1445769)2024.PubMed/NCBI View Article : Google Scholar | |
|
Xie Y, Zheng L, Chen W, Zeng Y, Yao K and Zhou T: Potential signal pathways and therapeutic effects of mesenchymal stem cell on oxidative stress in diseases. Curr Pharm Des. 31:83–94. 2025.PubMed/NCBI View Article : Google Scholar | |
|
Ajaz M, Singh I, Vugic L, Jani R, Rathnayake H, Diyapaththugama S, Mulaw GF and Colson NJ: The interplay of plant-based antioxidants, inflammation, and clinical outcomes in asthma: A systematic review. Respir Med. 236(107918)2025.PubMed/NCBI View Article : Google Scholar | |
|
Lewis BW, Ford ML, Rogers LK and Britt RD Jr: Oxidative stress promotes corticosteroid insensitivity in asthma and COPD. Antioxidants (Basel). 10(1335)2021.PubMed/NCBI View Article : Google Scholar | |
|
Michaeloudes C, Abubakar-Waziri H, Lakhdar R, Raby K, Dixey P, Adcock IM, Mumby S, Bhavsar PK and Chung KF: Molecular mechanisms of oxidative stress in asthma. Mol Aspects Med. 85(101026)2022.PubMed/NCBI View Article : Google Scholar | |
|
Sasaki H, Miyata J, Kawana A and Fukunaga K: Antiviral roles of eosinophils in asthma and respiratory viral infection. Front Allergy. 6(1548338)2025.PubMed/NCBI View Article : Google Scholar | |
|
Arora S, Naved T, Alam S, Chauhan B and Kalonia H: TLR 4/MD2 Complex inhibitors potential therapeutic prospective for asthma and asthma exacerbation. Res J Biotechnol. 16:164–176. 2021. | |
|
Ramu S, Calvén J, Michaeloudes C, Menzel M, Akbarshahi H, Chung KF and Uller L: TLR3/TAK1 signalling regulates rhinovirus-induced interleukin-33 in bronchial smooth muscle cells. ERJ Open Res. 6:00147–2020. 2020.PubMed/NCBI View Article : Google Scholar | |
|
Habib N, Pasha MA and Tang DD: Current understanding of asthma pathogenesis and biomarkers. Cells. 11(2764)2022.PubMed/NCBI View Article : Google Scholar | |
|
Savin IA, Zenkova MA and Sen'kova AV: Bronchial asthma, airway remodeling and lung fibrosis as successive steps of one process. Int J Mol Sci. 24(16042)2023.PubMed/NCBI View Article : Google Scholar | |
|
Rajvanshi N, Kumar P and Goyal JP: Global initiative for asthma guidelines 2024: An update. Indian Pediatr. 61:781–786. 2024.PubMed/NCBI | |
|
Finnerty JP, Hussain ABMA, Ponnuswamy A, Kamil HG and Abdelaziz A: Asthma and COPD as co-morbidities in patients hospitalised with Covid-19 disease: A global systematic review and meta-analysis. BMC Pulm Med. 23(462)2023.PubMed/NCBI View Article : Google Scholar | |
|
Kotecha EA, Fitzgerald DA and Kotecha S: Adherence in paediatric respiratory medicine: A review of the literature. Paediatr Respir Rev. 50:41–45. 2024.PubMed/NCBI View Article : Google Scholar | |
|
Toh MR, Ng GXZ, Goel I, Lam SW, Wu JT, Lee CF, Ong MEH, Matchar DB, Tan NC, Loo CM and Koh MS: Asthma prescribing trends, inhaler adherence and outcomes: A real-world data analysis of a multi-ethnic Asian asthma population. NPJ Prim Care Respir Med. 34(35)2024.PubMed/NCBI View Article : Google Scholar | |
|
Cardet JC, Papi A and Reddel HK: ‘As-needed’ inhaled corticosteroids for patients with asthma. J Allergy Clin Immunol Pract. 11:726–734. 2023.PubMed/NCBI View Article : Google Scholar | |
|
Cokorudy B, Harrison J and Chan AHY: Digital markers of asthma exacerbations: A systematic review. ERJ Open Res. 10:00014–2024. 2024.PubMed/NCBI View Article : Google Scholar | |
|
Tashiro H, Kuwahara Y, Kurihara Y and Takahashi K: Molecular mechanisms and clinical impact of biologic therapies in severe asthma. Respir Investig. 63:50–60. 2025.PubMed/NCBI View Article : Google Scholar | |
|
Aljohani AH, Alsufiani H and Ahmed G: Non-invasive management of severe subcutaneous emphysema in a pediatric asthma exacerbation: A case report and review. Int J Emerg Med. 17(203)2024.PubMed/NCBI View Article : Google Scholar | |
|
Ying Y, Khunthason S, Apidechkul T and Nilvarangkul K: Influencing factors of good quality of life among chronic obstructive pulmonary disease patients living in Zhejiang Province, China. Sci Rep. 14(8687)2024.PubMed/NCBI View Article : Google Scholar | |
|
Alforque RG and Murray B: The impact of microbiome supplementation on managing asthma exacerbations in adults. Irish J Med Sci. 193(S224)2024. | |
|
Moore E, Gassasse ZZ and Quint JK: Validating the recording of exacerbations of asthma in electronic health records: A systematic review protocol. BMJ Open. 14(e088849)2024.PubMed/NCBI View Article : Google Scholar | |
|
Petat H and Mazenq J: The impact of maternal smoking during pregnancy on respiratory disease in children. Rev Mal Respir. 41:768–775. 2024.PubMed/NCBI View Article : Google Scholar : (In French). | |
|
Li X, Yuan L and Wang F: Health outcomes of electronic cigarettes. Chin Med J (Engl). 137:1903–1911. 2024.PubMed/NCBI View Article : Google Scholar | |
|
Wills TA, Maziak W, Asfar T and Roy S: Current perspective on e-cigarette use and respiratory outcomes: Mechanisms and messaging. Expert Rev Respir Med. 18:597–609. 2024.PubMed/NCBI View Article : Google Scholar | |
|
Nielsen AO, Lange P, Hilberg O, Farver-Vestergaard I, Ibsen R and Løkke A: COPD and smoking status-it does matter: Characteristics and prognosis of COPD according to smoking status. Chronic Obstr Pulm Dis. 11:56–67. 2024.PubMed/NCBI View Article : Google Scholar | |
|
Annareddy S, Ghewade B, Jadhav U, Wagh P and Sarkar S: Unveiling the long-term lung consequences of smoking and tobacco consumption: A narrative review. Cureus. 16(e66415)2024.PubMed/NCBI View Article : Google Scholar | |
|
Tiotiu A, Ioan I, Wirth N, Romero-Fernandez R and González-Barcala FJ: The impact of tobacco smoking on adult asthma outcomes. Int J Environ Res Public Health. 18(992)2021.PubMed/NCBI View Article : Google Scholar | |
|
Tsikrika S, Dai S, Dilektasli A, Katsaounou P and Dagli E: Challenges and perspectives of tobacco cessation in special groups of patients and populations. Breathe (Sheff). 19(220224)2023.PubMed/NCBI View Article : Google Scholar | |
|
Bekmagambetova R, Kachiyeva Z, Ispayeva Z, Fakhradiyev I, Gotua M, Kenzhebekova R, Tolegenkyzy A, Kovaleva K, Turlugulova G, Zhakiyeva A, et al: Genetic associations with asthma in the Kazakh Population: A case-control study focusing on ACTN3 and TSBP1 polymorphisms. Georgian Med News. 188–194. 2024.PubMed/NCBI | |
|
Syssoyev D, Mussina K, Poddighe D, Gaipov A and Galiyeva D: All-cause hospital admissions and incidence of asthma in children in Kazakhstan: A population-based retrospective cohort study. Sci Rep. 15(8985)2025.PubMed/NCBI View Article : Google Scholar | |
|
Ispayeva Z, Bekmagambetova R, Mustafina M, Kovzel E, Tusupbekova G, Morenko M, Saliev T, Tanabayeva S and Fakhradiyev I: Reliability and validity of the Kazakh-language act questionnaire as an asthma control tool. Georgian Med News. 85–90. 2024.PubMed/NCBI | |
|
Aron J, Baldomero AK, Rau A, Fiecas MB, Wendt CH and Berman JD: Individual risk factors of PM2.5 associated with wintertime mortality in urban patients with COPD. Chest. 165:825–835. 2024.PubMed/NCBI View Article : Google Scholar | |
|
Ho TH, Dang CV, Pham TTB, Ngo HTT and Wangwongwatana S: Assessment of the association between PM2.5 concentration and hospital admissions for pediatric asthma in Ho Chi Minh City, Viet Nam. Hyg Environ Healh Adv. 11(100097)2024. | |
|
Chen S, Liu D, Huang L, Guo C, Gao X, Xu Z, Yang Z, Chen Y, Li M and Yang J: Global associations between long-term exposure to PM2.5 constituents and health: A systematic review and meta-analysis of cohort studies. J Hazard Mater. 474(134715)2024.PubMed/NCBI View Article : Google Scholar | |
|
Zanobetti A, Ryan PH, Coull BA, Luttmann-Gibson H, Datta S, Blossom J, Brokamp C, Lothrop N, Miller RL, Beamer PI, et al: Early-life exposure to air pollution and childhood asthma cumulative incidence in the ECHO CREW consortium. JAMA Netw Open. 7(e240535)2024.PubMed/NCBI View Article : Google Scholar | |
|
Charres I, Lucarelli F, Feliciano M, Furst L and Alves C: Seasonal variations of size-classified aerosol-bound elements in school environments and risk factors for the prevalence of atopic diseases among pupils. Build Environ. 265(111949)2024. | |
|
Patlán-Hernández AR, Savouré M, Audureau E, Monfort C, de Castro M, Epaud R, de Hoogh K, Hough I, Kloog I, Lanone S, et al: Associations of exposure to outdoor PM2.5 and NO2 during pregnancy with childhood asthma, rhinitis, and eczema in a predominantly rural French mother-child cohort. Environ Pollut. 363(125206)2024.PubMed/NCBI View Article : Google Scholar | |
|
Wassmer RW and Turgeon MD: Particulates matter: The influence of cumulative local air pollution exposure on sixth-grade academic achievement in California. Environ Health Insights. 18(11786302241293292)2024.PubMed/NCBI View Article : Google Scholar | |
|
Agache I, Annesi-Maesano I, Cecchi L, Biagioni B, Chung F, D'Amato G, Damialis A, Del Giacco S, Dominguez Ortega J, Galán C, et al: EAACI guidelines on environmental science for allergy and asthma-recommendations on the impact of indoor air pollutants on the risk of new-onset asthma and on asthma-related outcomes. Allergy. 80:651–676. 2025.PubMed/NCBI View Article : Google Scholar | |
|
Chatkin J, Correa L and Santos U: External environmental pollution as a risk factor for asthma. Clin Rev Allergy Immunol. 62:72–89. 2022.PubMed/NCBI View Article : Google Scholar | |
|
Paterson CA, Sharpe RA, Taylor T and Morrissey K: Indoor PM2.5, VOCs and asthma outcomes: A systematic review in adults and their home environments. Environ Res. 202(111631)2021.PubMed/NCBI View Article : Google Scholar | |
|
Emetere ME, Olaniyan IE, Fadiji JO, Olaogun KA, Adeniji NO, Deji-Jinadu BB and Olapade OT: Indoor air pollution: A review on the challenges in third world countries. Air Soil Water Res. 17:1–14. 2024. | |
|
Grant TL and Wood RA: The influence of urban exposures and residence on childhood asthma. Pediatr Allergy Immunol. 33(e13784)2022.PubMed/NCBI View Article : Google Scholar | |
|
Holden KA, Lee AR, Hawcutt DB and Sinha IP: The impact of poor housing and indoor air quality on respiratory health in children. Breathe (Sheff). 19(230058)2023.PubMed/NCBI View Article : Google Scholar | |
|
Agache I, Canelo-Aybar C, Annesi-Maesano I, Cecchi L, Biagioni B, Chung F, D'Amato G, Damialis A, Del Giacco S, De Las Vecillas L, et al: The impact of indoor pollution on asthma-related outcomes: A systematic review for the EAACI guidelines on environmental science for allergic diseases and asthma. Allergy. 79:1761–1788. 2024.PubMed/NCBI View Article : Google Scholar | |
|
Kang I, McCreery A, Azimi P, Gramigna A, Baca G, Hayes W, Crowder T, Scheu R, Evens A and Stephens B: Impacts of residential indoor air quality and environmental risk factors on adult asthma-related health outcomes in Chicago, IL. J Expo Sci Environ Epidemiol. 33:358–367. 2023.PubMed/NCBI View Article : Google Scholar | |
|
Vinnikov D, Rapisarda V, Babanov S, Vitale E, Strizhakov L, Romanova Z and Mukatova I: High levels of indoor fine particulate matter during the cold season in Almaty prompt urgent public health action. PLoS One. 18(e0285477)2023.PubMed/NCBI View Article : Google Scholar | |
|
Morales-Amparano MB, Teran MG, Huerta-Ocampo JÁ and Teran LM: Impact of enolase in allergic disease. Curr Allergy Asthma Rep. 24:571–579. 2024.PubMed/NCBI View Article : Google Scholar | |
|
Liu L, Li X, Sun Y and Li G: Allergen sensitization of parents and children with respiratory allergic diseases. Indian Pediatr. 61:730–734. 2024.PubMed/NCBI | |
|
Xu X, Li J, Zhang X, Xi L, Gao Y, Li X, Zhang Y and Zhang L: Blood and local eosinophil levels in chronic rhinitis: Observations during seasonal allergen exposure and non-exposure. World Allergy Organ J. 17(100930)2024.PubMed/NCBI View Article : Google Scholar | |
|
Sontakke A, Saxena P, Girdhar N, Ali S and Sarda A: Study of various phenotypes of bronchial asthma and skin sensitivity to common aeroallergens in allergic asthma patients. Alerg Astma Immunol. 29:100–104. 2024. | |
|
Mansoor J, Zia Ul Haq M, Ahsan Z, Bilal M and Fatima SS: Effect of high-efficiency particulate air filter on children with asthma: A systematic review protocol of RCTs. BMJ Open. 14(e087493)2024.PubMed/NCBI View Article : Google Scholar | |
|
Adibi A, Barn P, Shellington EM, Harvard S, Johnson KM and Carlsten C: High-efficiency particulate air filters for preventing wildfire-related asthma complications: A cost-effectiveness study. Am J Respir Crit Care Med. 209:175–184. 2024.PubMed/NCBI View Article : Google Scholar | |
|
Luedders J, Poole JA and Rorie AC: Extreme weather events and asthma. Immunol Allergy Clin North Am. 44:35–44. 2024.PubMed/NCBI View Article : Google Scholar | |
|
Makrufardi F, Manullang A, Rusmawatiningtyas D, Chung KF, Lin SC and Chuang HC: Extreme weather and asthma: A systematic review and meta-analysis. Eur Respir Rev. 32(230019)2023.PubMed/NCBI View Article : Google Scholar | |
|
Han A, Deng S, Yu J, Zhang Y, Jalaludin B and Huang C: Asthma triggered by extreme temperatures: From epidemiological evidence to biological plausibility. Environ Res. 216(114489)2023.PubMed/NCBI View Article : Google Scholar | |
|
Álvarez-Sánchez A, Córdova-Luspa LE and Pachacama-Freire MA: The climate in different tourist locations affecting children with bronchial asthma. In: Advances in Tourism, Technology and Systems. ICOTTS 2023. Smart Innovation, Systems and Technologies. Abreu A, Carvalho JV, Liberato P and Monroy HC (eds). Vol 383. Springer, Singapore, pp505-516, 2024. | |
|
Kuhn BT and Gupta R: Improving wildfire readiness among patients with chronic obstructive pulmonary disease and asthma: Applying a population health approach to climate change. Chronic Obstr Pulm Dis. 11:427–435. 2024.PubMed/NCBI View Article : Google Scholar | |
|
Gao J, Shen ZY, Štreimikienė D, Baležentis T and Zhou Y: Associating highway density with asthma: Unraveling the link between traffic-related pollution and health in U.S. non-california metropolitan areas. The Singapore Economic Review, 2024. | |
|
Galarneau JM, Beach J and Cherry N: Respiratory Ill-health and welding exposures: A canadian cohort study. Am J Ind Med. 68:99–111. 2025.PubMed/NCBI View Article : Google Scholar | |
|
Zivadinovic N, Jaoiun K, Klepaker G, Wagstaff A, Torén K, Henneberger PK, Kongerud J, Abrahamsen R and Fell AKM: Occupational exposure and new-onset asthma in the population-based Telemark study: A 5-year follow-up. BMJ Open. 14(e090131)2024.PubMed/NCBI View Article : Google Scholar | |
|
Yang L, Xinting C, Aie Z, Ruiqi X, Moreira P and Mei D: Insights into uncovered public health risks. The case of asthma attacks among archival workers: A cross-sectional study. Front Public Health. 12(1397236)2024.PubMed/NCBI View Article : Google Scholar | |
|
Pemberton MA, Arts JH and Kimber I: Identification of true chemical respiratory allergens: Current status, limitations and recommendations. Regul Toxicol Pharmacol. 147(105568)2024.PubMed/NCBI View Article : Google Scholar | |
|
Pinto MDS, Ribeiro CO, Morisco de Sá P, Castro HA, Bártholo TP, Lopes AJ and Melo PL: Oscillometry in asthma: Respiratory modeling and analysis in occupational and work-exacerbated phenotypes. J Asthma Allergy. 17:983–1000. 2024.PubMed/NCBI View Article : Google Scholar | |
|
Jo W, Seo KW, Jung HS, Park CY, Kang BJ, Kang HH, Ra SW, Jegal Y, Ahn JJ, Park SE, et al: Clinical importance of work-exacerbated asthma: Findings from a prospective asthma cohort in a highly industrialized City in Korea. Allergy Asthma Immunol Res. 13:256–270. 2021.PubMed/NCBI View Article : Google Scholar | |
|
Roio LCD, Stelmach R, Mizutani RF, Terra-Filho M and Santos UDP: Work-related asthma consequences on socioeconomic, asthma control, quality of life, and psychological status compared with non-work-related asthma: A cross-sectional study in an upper-middle-income country. Am J Ind Med. 66:529–539. 2023.PubMed/NCBI View Article : Google Scholar | |
|
Kongsupon N, Walters GI, Adab P and Jordan RE: Screening tools for work-related asthma and their diagnostic accuracy: A systematic review protocol. BMJ Open. 12(e058054)2022.PubMed/NCBI View Article : Google Scholar | |
|
Alpaydin AO, Bora M, Yorgancioglu A, Coskun AS and Celik P: Asthma control test and asthma quality of life questionnaire association in adults. Iran J Allergy Asthma Immunol. 11:301–307. 2012.PubMed/NCBI | |
|
Gerlich J, Ohlander J, Kromhout H, Vermeulen R, Söhler S, Radon K, Nowak D, Karrasch S, Adaskina N, Vogelmeier C, et al: Cumulative occupational exposure to gases and fumes is associated with impairment in lung function and disease-related quality of life in a German COPD patient cohort. Occup Environ Med. 81:26–33. 2023.PubMed/NCBI View Article : Google Scholar | |
|
Lantto J, Suojalehto H and Lindström I: Long-term outcome of occupational asthma from irritants and low-molecular-weight sensitizers. J Allergy Clin Immunol Pract. 11:1224–1232.e2. 2023.PubMed/NCBI View Article : Google Scholar | |
|
Luo L, Tang J, Du X and Li N: Chronic obstructive pulmonary disease and the airway microbiome: A review for clinicians. Respir Med. 225(107586)2024.PubMed/NCBI View Article : Google Scholar | |
|
Sherris AR, Hazlehurst MF, Dearborn LC, Loftus CT, Szpiro AA, Adgent MA, Carroll KN, Day DB, LeWinn KZ, Ni Y, et al: Prenatal exposure to ambient fine particulate matter and child lung function in the CANDLE cohort. Ann Med. 56(2422051)2024.PubMed/NCBI View Article : Google Scholar | |
|
Mermiri M, Mavrovounis G, Kanellopoulos N, Papageorgiou K, Spanos M, Kalantzis G, Saharidis G, Gourgoulianis K and Pantazopoulos I: Effect of PM2.5 levels on ED visits for respiratory causes in a Greek semi-urban area. J Pers Med. 12(1849)2022.PubMed/NCBI View Article : Google Scholar | |
|
Zhang Y, Yin X and Zheng X: The relationship between PM2.5 and the onset and exacerbation of childhood asthma: A short communication. Front Pediatr. 11(1191852)2023.PubMed/NCBI View Article : Google Scholar | |
|
Pai SJ, Carter TS, Heald CL and Kroll JH: Updated World Health Organization air quality guidelines highlight the importance of non-anthropogenic PM2.5. Environ Sci Technol Lett. 9:501–506. 2022.PubMed/NCBI View Article : Google Scholar | |
|
Ababio BA, Ashong GW, Agyekum TP, Yeboah BA, Nkansah MA, Hogarh JN, Commeh MK, Kwaansa-Ansah EE, Dabie K, Adulley F, et al: Comprehensive health risk assessment of urban ambient air pollution (PM2.5, NO2 and O3) in Ghana. Ecotoxicol Environ Saf. 289(117591)2025.PubMed/NCBI View Article : Google Scholar | |
|
Rentschler J and Leonova N: Global air pollution exposure and poverty. Nat Commun. 14(4432)2023.PubMed/NCBI View Article : Google Scholar | |
|
Wang J, Cortes-Ramirez J, Gan T, Davies JM and Hu W: Effects of climate and environmental factors on childhood and adolescent asthma: A systematic review based on spatial and temporal analysis evidence. Sci Total Environ. 951(175863)2024.PubMed/NCBI View Article : Google Scholar | |
|
Rorie A and Poole JA: The role of extreme weather and climate-related events on asthma outcomes. Immunol Allergy Clin North Am. 41:73–84. 2021.PubMed/NCBI View Article : Google Scholar | |
|
Bolan S, Sharma S, Mukherjee S, Gomez Isaza DF, Rodgers EM, Zhou P, Hou D, Scordo F, Chandra S, Siddique KHM and Bolan N: Wildfires under changing climate, and their environmental and health impacts. J Soils Sediments. 599–600. 2025. | |
|
Chen G, Qiu M, Wang P, Zhang Y, Shindell D and Zhang H: Continuous wildfires threaten public and ecosystem health under climate change across continents. Front Environ Sci Eng. 18(130)2024. | |
|
Marando F, Heris MP, Zulian G, Udías A, Mentaschi L, Chrysoulakis N, Parastatidis D and Maes J: Urban heat island mitigation by green infrastructure in European functional urban areas. Sustain Cities Soc. 77(103564)2022. | |
|
Wu Q, Huang Y, Irga P, Kumar P, Li W, Wei W, Shon HK, Lei C and Zhou JL: Synergistic control of urban heat island and urban pollution island effects using green infrastructure. J Environ Manage. 370(122985)2024.PubMed/NCBI View Article : Google Scholar | |
|
Kennedy CT, Scotland GS, Cotton S and Turner SW: Direct and indirect costs of paediatric asthma in the UK: A cost analysis. Arch Dis Child. 109:724–729. 2024.PubMed/NCBI View Article : Google Scholar | |
|
Roberts MH, Duh MS, Rothnie KJ, Zhang S, Czira A, Slade D and Cheng WY: Thompson-Leduc P, Greatsinger A, Zhang A and Mapel D: Development and validation of a claims-based algorithm to identify moderate exacerbations in patients with asthma treated in the US. Respir Med. 226(107630)2024.PubMed/NCBI View Article : Google Scholar | |
|
Bruzzese JM, Céspedes A, Ainapudi V, Kingston S, Santana J and Zhao Y: Identification of barriers to seeing a healthcare provider among rural adolescents with poorly controlled asthma. Am J Respir Crit Care Med. 209(A6609)2024. | |
|
Choy A, Shellington EM, Collins-Fairclough A, Strydom N and Carlsten C: Geographic differences in availability and access to care services for asthma and COPD: Case study of vancouver coastal health, British Columbia. Can Respir J. 2024(8019557)2024.PubMed/NCBI View Article : Google Scholar | |
|
Bocian IY, Chin AR, Rodriguez A, Collins W, Sindher SB and Chinthrajah RS: Asthma management in the digital age. Front Allergy. 5(1451768)2024.PubMed/NCBI View Article : Google Scholar | |
|
Baker JA, Cardona ML and Brennan LD: Downstream effects of market changes on inhalers: Impacts on individuals with chronic lung disease. Respir Care. 69:1448–1456. 2024.PubMed/NCBI View Article : Google Scholar | |
|
Bourdin A, Bardin P and Chanez P: Imagining the severe asthma decision trees of the future. Expert Rev Respir Med. 18:561–567. 2024.PubMed/NCBI View Article : Google Scholar | |
|
Chen W, Puttock EJ, Schatz M, Crawford W, Vollmer WM, Xie F, Xu S, Lustigova E and Zeiger RS: Risk factors for acute asthma exacerbations in adults with mild asthma. J Allergy Clin Immunol Pract. 12:2705–2716.e6. 2024.PubMed/NCBI View Article : Google Scholar | |
|
Awwad O, AlMuhaissen S, Jalil MA, Battah Z, Hammour KA and Almonayer S: Impact of COVID-19 on asthma and COPD patients' hospital care: A lesson for future pandemics. J Pharm Health Serv Res. 15(rmae009)2024. | |
|
Dabbs W, Bradley MH and Chamberlin SM: Acute asthma exacerbations: Management strategies. Am Fam Physician. 109:43–50. 2024.PubMed/NCBI | |
|
Leukel PJ, Piette JD and Lee AA: Impact of loneliness and social support on acute health service use and symptom exacerbation among adults with asthma and COPD. J Clin Psychol Med Settings. 32:375–384. 2025.PubMed/NCBI View Article : Google Scholar | |
|
Hauerslev M, Alon K, Brustad N and Chawes B: Risk factors for nonattendance among children with asthma: A systematic review and meta-analysis. J Allergy Clin Immunol Pract. 12:2381–2389.e11. 2024.PubMed/NCBI View Article : Google Scholar | |
|
Guarnieri G, Olivieri B, Latorre M, Rizzi A, Blasi F, Canonica GW, Heffler E, Paggiaro P, Senna G and Caminati M: SANI study group. Asthma severity: The patient's point of view. Eur Clin Respir J. 11(2381307)2024.PubMed/NCBI View Article : Google Scholar | |
|
Tafere C, Bahiru B, Yehualaw A, Demsie DG, Feyisa K, Yismaw MB, Aschale E, Debasu Z, Yilma Z, Agmassie Z, et al: Medication non-adherence and predictor factors among adult asthmatic patients in Ethiopia: A systematic review and meta-analysis. J Asthma. 61:1109–1120. 2024.PubMed/NCBI View Article : Google Scholar | |
|
Román-Rodríguez M, McMullan I, Warner M, Compton CH, Tal-Singer R, Orlow JM and Han MK: Perspectives on treatment decisions, preferences, and adherence and long-term management in asthma and COPD: A qualitative analysis of patient, caregiver, and healthcare provider insights. Patient Prefer Adherence. 18:2295–2306. 2024.PubMed/NCBI View Article : Google Scholar | |
|
Murugaiya S, Murugesan B and S P: Prevalence and factors affecting the optimal and non-optimal peak inspiratory flow rate in stable and exacerbation phases of chronic obstructive pulmonary disease and bronchial asthma in India. Cureus. 16(e58670)2024.PubMed/NCBI View Article : Google Scholar | |
|
Halpin DMG and Mahler DA: Systematic review of the effects of patient errors using inhaled delivery systems on clinical outcomes in COPD. BMJ Open Respir Res. 11(e002211)2024.PubMed/NCBI View Article : Google Scholar | |
|
Carvalho D: Access from healthcare professionals to evidence-based pharmacotherapy in allergy management. Curr Opin Allergy Clin Immunol. 24:274–279. 2024.PubMed/NCBI View Article : Google Scholar | |
|
Al-Halbouni L, Ryan GW, Radu S, Spano M, Sabnani R, Phipatanakul W, Gerald LB, Garg A, Pbert L and Trivedi M: Exploring the relationship between school-supervised asthma therapy and social determinants of health in pediatric asthma care. Pediatr Pulmonol. 59:2553–2562. 2024.PubMed/NCBI View Article : Google Scholar | |
|
Amjad S, Tromburg C, Adesunkanmi M, Mawa J, Mahbub N, Campbell S, Chari R, Rowe BH and Ospina MB: Social determinants of health and pediatric emergency department outcomes: A systematic review and meta-analysis of observational studies. Ann Emerg. 83:291–313. 2024.PubMed/NCBI View Article : Google Scholar | |
|
Yohannes AM: Psychosocial support in pulmonary rehabilitation. Respir Care. 69:664–677. 2024.PubMed/NCBI View Article : Google Scholar | |
|
Sharrad KJ, Sanwo O, Cuevas-Asturias S, Kew KM, Carson-Chahhoud KV and Pike KC: Psychological interventions for asthma in children and adolescents. Cochrane Database Syst Rev. 1(CD013420)2024.PubMed/NCBI View Article : Google Scholar | |
|
Nicholas DB, Katz SL, Ciesielski J and Zulla RT: Psychosocial and service delivery impacts of the COVID-19 pandemic on children with respiratory conditions, their parents and their health care providers. Inquiry. 61(469580241246338)2024.PubMed/NCBI View Article : Google Scholar | |
|
Hung CT and Hung YC: Telemedicine use among adults with asthma in the United States, 2021-2022. Telemed J E Health. 30:1580–1587. 2024.PubMed/NCBI View Article : Google Scholar | |
|
Aggelidis X, Kritikou M, Makris M, Miligkos M, Papapostolou N, Papadopoulos NG and Xepapadaki P: Tele-monitoring applications in respiratory allergy. J Clin Med. 13(898)2024.PubMed/NCBI View Article : Google Scholar | |
|
Jafleh EA, Alnaqbi FA, Almaeeni HA, Faqeeh S, Alzaabi MA and Al Zaman K: The role of wearable devices in chronic disease monitoring and patient care: A comprehensive review. Cureus. 16(e68921)2024.PubMed/NCBI View Article : Google Scholar | |
|
Faiçal AVB, Mota LR, Correia DA, Monteiro LP, Souza EL and Terse-Ramos R: Telehealth for children and adolescents with chronic pulmonary disease: Systematic review. Rev Paul Pediatr. 42(e2024111)2023.PubMed/NCBI View Article : Google Scholar | |
|
Suvarna KC, Kumar P, Singh K, Kumar J and Goyal JP: Comparison of telemedicine versus in-person visit for control of asthma in children aged 7-17 years: A randomized controlled trial. Indian J Pediatr. 92:467–473. 2025.PubMed/NCBI View Article : Google Scholar | |
|
Alcoceba-Herrero I, Coco-Martín MB, Jiménez-Pérez JM, Leal-Vega L, Martín-Gutiérrez A, Dueñas-Gutiérrez C, Miramontes-González JP, Corral-Gudino L, de Castro-Rodríguez F, Royuela-Ruiz P and Arenillas-Lara JF: Randomized controlled trial to assess the feasibility of a novel clinical decision support system based on the automatic generation of alerts through remote patient monitoring. J Clin Med. 13(5974)2024.PubMed/NCBI View Article : Google Scholar | |
|
Cabrerizo-Carreño H, Muñoz-Esquerre M, Santos Pérez S, Romero-Ortiz AM, Fabrellas N and Guix-Comellas EM: Impact of the implementation of a telemedicine program on patients diagnosed with asthma. BMC Pulm Med. 24(32)2024.PubMed/NCBI View Article : Google Scholar | |
|
El Abed H, Ait-Taleb Lahsen H, El Malki H, Erraji AE, Benjelloun MC, Ragala MEA and Halim K: Factors associated with health-related quality of life in Moroccan adults with asthma. Asian J Soc Health Behav. 7:189–196. 2024. | |
|
Toyran M, Yagmur IT, Guvenir H, Haci IA, Bahceci S, Batmaz SB, Topal OY, Celik IK, Karaatmaca B, Misirlioglu ED, et al: Asthma control affects school absence, achievement and quality of school life: A multicenter study. Allergol Immunopathol (Madr). 48:545–552. 2020.PubMed/NCBI View Article : Google Scholar | |
|
Bhattacharya A, Syamlal G and Dodd KE: Medical costs and incremental medical costs of asthma among workers in the United States. Am J Ind Med. 67:834–843. 2024.PubMed/NCBI View Article : Google Scholar | |
|
Mahin M, Warner M, Dottin M, Olsen N and Marshall ET: Projected cost savings of a community health worker model for asthma home visits in the massachusetts pediatric medicaid population. Prev Chronic Dis. 21(E69)2024.PubMed/NCBI View Article : Google Scholar | |
|
Pakkasela J, Salmela P, Juntunen P, Karjalainen J and Lehtimäki L: Adherence to treatment guidelines and good asthma control in Finland. Eur Clin Respir J. 10(2149918)2022.PubMed/NCBI View Article : Google Scholar | |
|
Jaakkola MS, Aalto SAM, Hyrkäs-Palmu H and Jaakkola JJK: Association between regular exercise and asthma control among adults: The population-based Northern Finnish asthma study. PLoS One. 15(e0227983)2020.PubMed/NCBI View Article : Google Scholar | |
|
Thamboo AV, Lee M, Bhutani M, Chan C, Chan Y, Chapman KR, Chin CJ, Connors L, Dorscheid D, Ellis AK, et al: Canadian multidisciplinary expert consensus on the use of biologics in upper airways: A Delphi study. J Otolaryngol Head Neck Surg. 52(30)2023.PubMed/NCBI View Article : Google Scholar | |
|
Dong Y, Liu H and Zheng T: Association between Green space structure and the prevalence of asthma: A case study of toronto. Int J Environ Res Public Health. 18(5852)2021.PubMed/NCBI View Article : Google Scholar | |
|
Mtibaa M, Gupta S, Muthukumar M, Marvel J, Kaur H, Ishikawa R and Olivenstein R: Cost-effectiveness of once-daily, single-inhaler indacaterol acetate/glycopyrronium bromide/mometasone furoate in patients with uncontrolled moderate-to-severe asthma in Canada. Clinicoecon Outcomes Res. 13:957–967. 2021.PubMed/NCBI View Article : Google Scholar | |
|
Ledda AG, Can Bostan O and Del Giacco S: Telemedicine and remote monitoring in asthma care: Innovations triggered by the pandemic. Explor Asthma Allergy. 3(100974)2025. | |
|
Persaud YK: Using telemedicine to care for the asthma patient. Curr Allergy Asthma Rep. 22:43–52. 2022.PubMed/NCBI View Article : Google Scholar | |
|
Chang TM, Chen Y, Yang KD, Wang JY, Lin CY, Chang YJ, Chen CH and Tsai YG: Asthma control associated with anxiety and depression in asthmatic children following post-acute COVID-19. Pediatr Allergy Immunol. 35(e14168)2024.PubMed/NCBI View Article : Google Scholar | |
|
Thiel PS, Bougie O, Pudwell J, Shellenberger J, Velez MP and Murji A: Endometriosis and mental health: A population-based cohort study. Am J Obstet Gynecol. 230:649.e1–649.e19. 2024.PubMed/NCBI View Article : Google Scholar | |
|
Han YY and Celedón JC: The effects of violence and related stress on asthma. Ann Allergy Asthma Immunol. 133:630–640. 2024.PubMed/NCBI View Article : Google Scholar | |
|
Kollin SR, Clayton CK, Green VA and Lee AA: Emotion regulation among adults with asthma: Links with short-acting inhaler medication overuse and utilization of acute medical care. J Asthma. 62:481–491. 2025.PubMed/NCBI View Article : Google Scholar | |
|
Caulfield JI: Anxiety, depression, and asthma: New perspectives and approaches for psychoneuroimmunology research. Brain Behav Immun Health. 18(100360)2021.PubMed/NCBI View Article : Google Scholar | |
|
Mohd Tamil A, Ismail NH, Jaafar MH, Md Isa Z, Ismail R, Mat Nasir N, Miskan M, Zainol Abidin N, Ab Razak NH, Joundi R and Yusof KH: Depressive symptoms among adults: Baseline findings of PURE Malaysia cohort study. Heliyon. 10(e23042)2023.PubMed/NCBI View Article : Google Scholar | |
|
Patel NB, Céspedes A, Liu J and Bruzzese JM: Depressive symptoms are related to asthma control but not self-management among rural adolescents. Front Allergy. 4(1271791)2024.PubMed/NCBI View Article : Google Scholar | |
|
Tran L, Sharrad K, Kopsaftis Z, Stallman HM, Tai A, Spurrier N, Esterman A and Carson-Chahhoud K: Pharmacological interventions for the treatment of psychological distress in patients with asthma: A systematic review and meta-analysis. J Asthma. 58:759–769. 2021.PubMed/NCBI View Article : Google Scholar | |
|
Shi Y and Han Q: Does maternal anxiety and depression increase the risk of asthma in the offspring? A systematic review and meta-analysis. Eur Rev Med Pharmacol Sci. 28:1066–1076. 2024.PubMed/NCBI View Article : Google Scholar | |
|
Ye G, Baldwin DS and Hou R: Anxiety in asthma: A systematic review and meta-analysis. Psychol Med. 51:11–20. 2021.PubMed/NCBI View Article : Google Scholar | |
|
Rolland-Debord C, Goriounov I and Pitron V: The psychological burden of asthma. Rev Mal Respir. 38:721–732. 2021.PubMed/NCBI View Article : Google Scholar : (In French). | |
|
Grover N, Kumaraiah V, Prasadrao PS and D'souza G: Cognitive behavioural intervention in bronchial asthma. J Assoc Physicians India. 50:896–900. 2002.PubMed/NCBI | |
|
Yohannes AM: Anxiety and post-traumatic stress disorders in patients with chronic respiratory diseases. Curr Opin Support Palliat Care. 17:290–295. 2023.PubMed/NCBI View Article : Google Scholar | |
|
Pateraki E and Morris PG: Effectiveness of cognitive behavioural therapy in reducing anxiety in adults and children with asthma: A systematic review. J Asthma. 55:532–554. 2018.PubMed/NCBI View Article : Google Scholar | |
|
Bajpai A: Hypothalamic-pituitary-adrenal axis suppression with inhaled corticosteroids-time to close the debate? Indian J Pediatr. 91:426–427. 2024.PubMed/NCBI View Article : Google Scholar | |
|
Vafaee F, Shirzad S, Shamsi F and Boskabady MH: Neuroscience and treatment of asthma, new therapeutic strategies and future aspects. Life Sci. 292(120175)2022.PubMed/NCBI View Article : Google Scholar | |
|
Palumbo ML, Prochnik A, Wald MR and Genaro AM: Chronic stress and glucocorticoid receptor resistance in asthma. Clin Ther. 42:993–1006. 2020.PubMed/NCBI View Article : Google Scholar | |
|
Drake MG, Cook M, Fryer AD, Jacoby DB and Scott GD: Airway sensory nerve plasticity in asthma and chronic cough. Front Physiol. 12(720538)2021.PubMed/NCBI View Article : Google Scholar | |
|
Jaramillo AM, Harder AQ, Holguin F and Evans CM: Vagal reflexes in airway hyperreactivity: Novel pathways and a note of caution for studies in mice. Am J Respir Cell Mol Biol. 68:231–233. 2023.PubMed/NCBI View Article : Google Scholar | |
|
Patella V, Pelaia C, Zunno R and Pelaia G: Biologicals decrease psychological distress, anxiety and depression in severe asthma, despite Covid-19 pandemic. Respir Med. 200(106916)2022.PubMed/NCBI View Article : Google Scholar | |
|
Beyhan Sagmen S, Yildizeli SO, Baykan H, Ozdemir M and Ceyhan B: The effects of anxiety and depression on asthma control and their association with strategies for coping with stress and social acceptance. Rev Fr Allergol. 60:401–406. 2020. | |
|
Stubbs MA, Clark VL, Gibson PG, Yorke J and McDonald VM: Associations of symptoms of anxiety and depression with health-status, asthma control, dyspnoea, dysfunction breathing and obesity in people with severe asthma. Respir Res. 23(341)2022.PubMed/NCBI View Article : Google Scholar | |
|
Buican IL, Gheorman V, Udriştoiu I, Olteanu M, Rădulescu D, Calafeteanu DM, Nemeş AF, Călăraşu C, Rădulescu PM and Streba CT: Interactions between cognitive, affective, and respiratory profiles in chronic respiratory disorders: A cluster analysis approach. Diagnostics (Basel). 14(1153)2024.PubMed/NCBI View Article : Google Scholar | |
|
Roberts M, Smith T, Wheatley J and Cho JG: Symptom burden of patients with chronic obstructive pulmonary disease attending the westmead breathlessness service: Prevalence, associations, and sex-related differences. Int J Chron Obstruct Pulmon Dis. 18:2825–2837. 2023.PubMed/NCBI View Article : Google Scholar | |
|
Jarjour IT, Jarjour LK, Tran K and Czyzewski D: Functional syncope in children and adolescents: A retrospective cohort study. Pediatr Neurol. 162:21–27. 2025.PubMed/NCBI View Article : Google Scholar | |
|
Sharrad K, Martini C, Tai A, Spurrier N, Smith R, Esterman A, Gwilt I, Sandford D and Carson-Chahhoud K: Mixed reality technology to deliver psychological interventions to adolescents with asthma: Qualitative study using the theoretical framework of acceptability. JMIR Hum Factors. 10(e34629)2023.PubMed/NCBI View Article : Google Scholar | |
|
AL-Awaisheh RI, IA AB and E AG: Evaluation of the prevalence of anxiety and depression and the impact of asthma control level on these parameters among asthmatic patients. Pharm Pract (Granada). 22:1–8. 2024. | |
|
Bouloukaki I, Christodoulakis A, Margetaki K and Tsiligianni I: The effect of sleep impairment, as assessed by the CASIS questionnaire, in patients with chronic obstructive pulmonary disease on disease severity and physical and mental health: A cross-sectional study in primary care. Biomedicines. 12(1644)2024.PubMed/NCBI View Article : Google Scholar |