Blood‑brain barrier dysfunction in epilepsy: Mechanisms, therapeutic strategies and future orientation (Review)
- Authors:
- Na Huang
- Yawen Huang
- Zhenyuan Deng
- Shuya Qi
- Wei Zhang
- Yuanyuan Liu
- Guohe Tan
-
Affiliations: Institute of Neuroscience and Guangxi Key Laboratory of Brain Science, Department of Human Anatomy, School of Basic Medical Sciences, Guangxi Medical University, Nanning, Guangxi Zhuang Autonomous Region 530016, P.R. China, Guangxi Key Laboratory of Regenerative Medicine, Collaborative Innovation Centre of Regenerative Medicine and Medical BioResource Development and Application Co‑constructed by the Province and Ministry, Nanning, Guangxi Zhuang Autonomous Region 530016, P.R. China - Published online on: July 3, 2025 https://doi.org/10.3892/ijmm.2025.5577
- Article Number: 136
-
Copyright: © Huang et al. This is an open access article distributed under the terms of Creative Commons Attribution License.
This article is mentioned in:
Abstract
 |
 |
 |
 |
 |
 |
|
Thijs RD, Surges R, O'Brien TJ and Sander JW: Epilepsy in adults. Lancet. 393:689–701. 2019. View Article : Google Scholar : PubMed/NCBI | |
|
World Health Organization: Epilepsy: A public health imperative: Summary. World Health Organization; 2019 | |
|
Shao LR, Habela CW and Stafstrom CE: Pediatric epilepsy mechanisms: Expanding the paradigm of excitation/inhibition imbalance. Children (Basel). 6:232019.PubMed/NCBI | |
|
Fisher RS, Cross JH, French JA, Higurashi N, Hirsch E, Jansen FE, Lagae L, Moshé SL, Peltola J, Roulet Perez E, et al: Operational classification of seizure types by the international league against epilepsy: Position paper of the ILAE commission for classification and terminology. Epilepsia. 58:522–530. 2017. View Article : Google Scholar : PubMed/NCBI | |
|
Chen Z, Brodie MJ, Liew D and Kwan P: Treatment outcomes in patients with newly diagnosed epilepsy treated with established and new antiepileptic drugs: A 30-year longitudinal cohort study. JAMA Neurol. 75:279–286. 2018. View Article : Google Scholar : | |
|
Cendes F, Sakamoto AC, Spreafico R, Bingaman W and Becker AJ: Epilepsies associated with hippocampal sclerosis. Acta Neuropathol. 128:21–37. 2014. View Article : Google Scholar : PubMed/NCBI | |
|
Liu X, Zhang Y, Zhao Y, Zhang Q and Han F: The neurovascular unit dysfunction in the molecular mechanisms of epileptogenesis and targeted therapy. Neurosci Bull. 40:621–634. 2024. View Article : Google Scholar : PubMed/NCBI | |
|
Devinsky O, Vezzani A, O'Brien TJ, Jette N, Scheffer IE, de Curtis M and Perucca P: Epilepsy Nat Rev Dis Primers. 4:180242018. View Article : Google Scholar | |
|
Sultana B, Panzini MA, Veilleux Carpentier A, Comtois J, Rioux B, Gore G, Bauer PR, Kwon CS, Jetté N, Josephson CB and Keezer MR: Incidence and prevalence of drug-resistant epilepsy: A systematic review and meta-analysis. Neurology. 96:805–817. 2021. View Article : Google Scholar : PubMed/NCBI | |
|
Kantanen AM, Reinikainen M, Parviainen I and Kälviäinen R: Long-term outcome of refractory status epilepticus in adults: A retrospective population-based study. Epilepsy Res. 133:13–21. 2017. View Article : Google Scholar : PubMed/NCBI | |
|
Strzelczyk A, Griebel C, Lux W, Rosenow F and Reese JP: The Burden of severely drug-refractory epilepsy: A comparative longitudinal evaluation of mortality, morbidity, resource use, and cost using german health insurance data. Front Neurol. 8:7122017. View Article : Google Scholar | |
|
Wang T, Wang J, Dou Y, Yan W, Ding D, Lu G, Ma J, Zhou Y, Li T, Zhou S, et al: Clinical characteristics and prognosis in a large paediatric cohort with status epilepticus. Seizure. 80:5–11. 2020. View Article : Google Scholar : PubMed/NCBI | |
|
Tian L, Li Y, Xue X, Wu M, Liu F, Hao X and Zhou D: Super-refractory status epilepticus in West China. Acta Neurol Scand. 132:1–6. 2015. View Article : Google Scholar | |
|
Al-Otaibi FA, Hamani C and Lozano AM: Neuromodulation in epilepsy. Neurosurgery. 69:957–979. 2011. View Article : Google Scholar : PubMed/NCBI | |
|
Dadas A and Janigro D: Breakdown of blood brain barrier as a mechanism of post-traumatic epilepsy. Neurobiol Dis. 123:20–26. 2019. View Article : Google Scholar : | |
|
Baghirov H: Receptor-mediated transcytosis of macromolecules across the blood-brain barrier. Expert Opin Drug Deliv. 20:1699–1711. 2023. View Article : Google Scholar : PubMed/NCBI | |
|
Chaves JCS, Dando SJ, White AR and Oikari LE: Blood-brain barrier transporters: An overview of function, dysfunction in Alzheimer's disease and strategies for treatment. Biochim Biophys Acta Mol Basis Dis. 1870:1669672024. View Article : Google Scholar | |
|
Patabendige A and Janigro D: The role of the blood-brain barrier during neurological disease and infection. Biochem Soc Trans. 51:613–626. 2023. View Article : Google Scholar : PubMed/NCBI | |
|
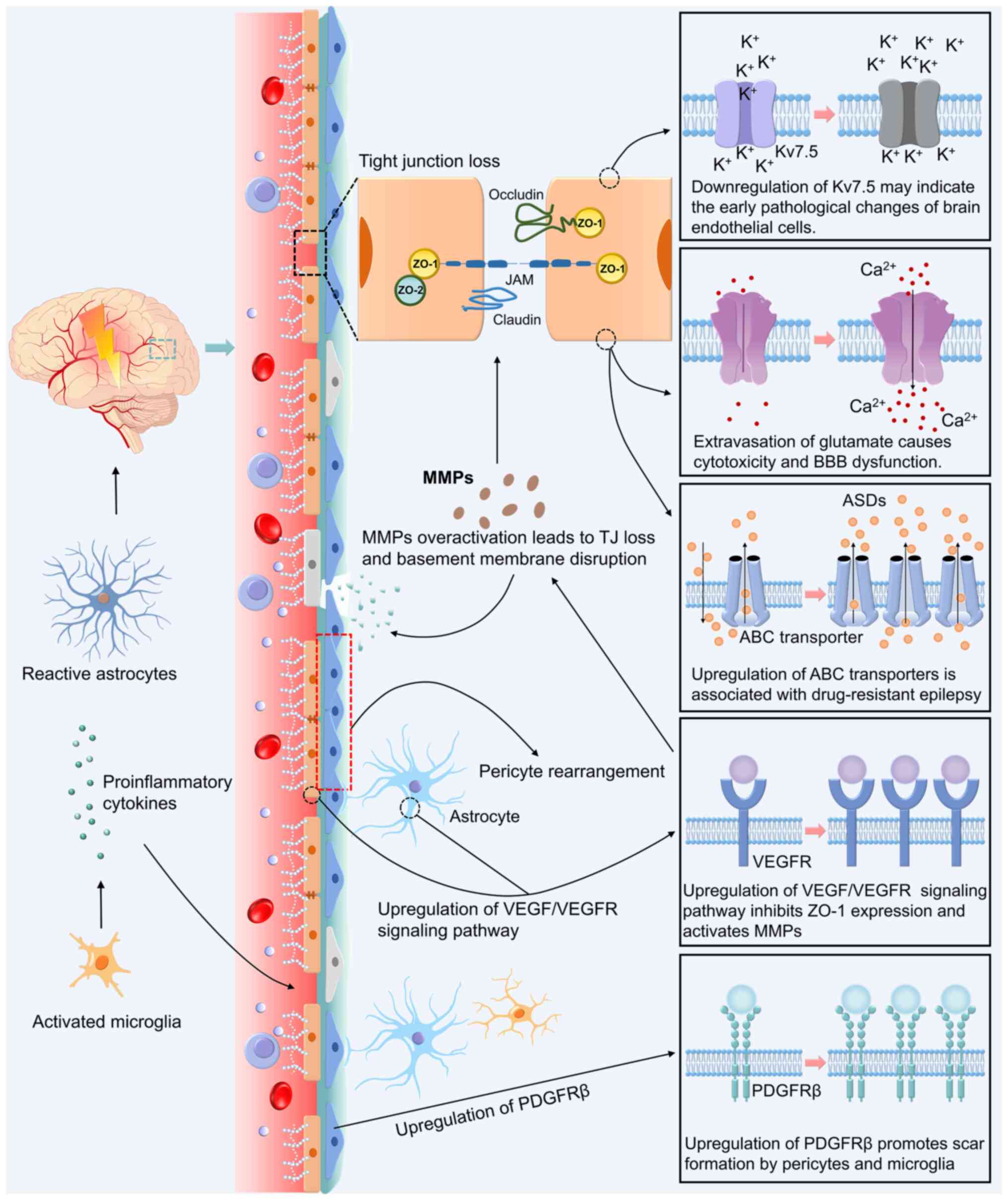
Vazana U, Veksler R, Pell GS, Prager O, Fassler M, Chassidim Y, Roth Y, Shahar H, Zangen A, Raccah R, et al: Glutamate-mediated blood-brain barrier opening: Implications for neuroprotection and drug delivery. J Neurosci. 36:7727–7739. 2016. View Article : Google Scholar : PubMed/NCBI | |
|
Leandro K, Bicker J, Alves G, Falcão A and Fortuna A: ABC transporters in drug-resistant epilepsy: Mechanisms of upregulation and therapeutic approaches. Pharmacol Res. 144:357–376. 2019. View Article : Google Scholar : PubMed/NCBI | |
|
Celentano C, Carotenuto L, Miceli F, Carleo G, Corrado B, Baroli G, Iervolino S, Vecchione R, Taglialatela M and Barrese V: Kv7 channel activation reduces brain endothelial cell permeability and prevents kainic acid-induced blood-brain barrier damage. Am J Physiol Cell Physiol. 326:C893–C904. 2024. View Article : Google Scholar : PubMed/NCBI | |
|
Reimann F: Liver diseases and pernicious anemia; clinical and physiopathological study of the behavior of the anti-pernicious factor in the body. Blut. 4:261–279. 1958.In German. View Article : Google Scholar : PubMed/NCBI | |
|
Bentivoglio M and Kristensson K: Tryps and trips: Cell trafficking across the 100-year-old blood-brain barrier. Trends Neurosci. 37:325–333. 2014. View Article : Google Scholar : PubMed/NCBI | |
|
Reese TS and Karnovsky MJ: Fine structural localization of a blood-brain barrier to exogenous peroxidase. J Cell Biol. 34:207–217. 1967. View Article : Google Scholar : PubMed/NCBI | |
|
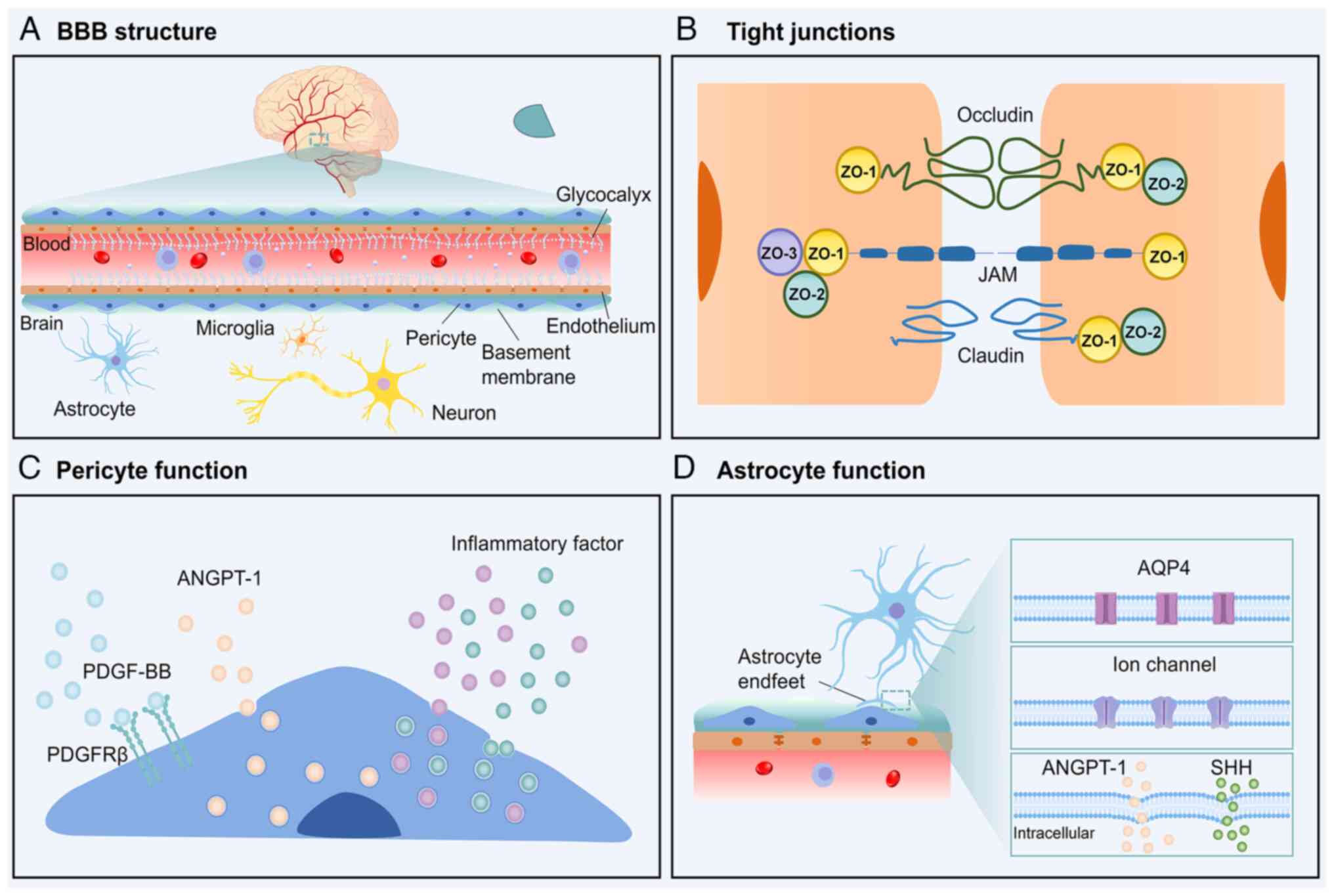
Zhang S, Gan L, Cao F, Wang H, Gong P, Ma C, Ren L, Lin Y and Lin X: The barrier and interface mechanisms of the brain barrier, and brain drug delivery. Brain Res Bull. 190:69–83. 2022. View Article : Google Scholar : PubMed/NCBI | |
|
Yan L, Moriarty RA and Stroka KM: Recent progress and new challenges in modeling of human pluripotent stem cell-derived blood-brain barrier. Theranostics. 11:10148–10170. 2021. View Article : Google Scholar : PubMed/NCBI | |
|
Ushiyama A, Kataoka H and Iijima T: Glycocalyx and its involvement in clinical pathophysiologies. J Intensive Care. 4:592016. View Article : Google Scholar : PubMed/NCBI | |
|
Iba T and Levy JH: Derangement of the endothelial glycocalyx in sepsis. J Thromb Haemost. 17:283–294. 2019. View Article : Google Scholar | |
|
Liu R, Collier JM, Abdul-Rahman NH, Capuk O, Zhang Z and Begum G: Dysregulation of Ion channels and transporters and blood-brain barrier dysfunction in Alzheimer's disease and vascular dementia. Aging Dis. 15:1748–1770. 2024.PubMed/NCBI | |
|
Nguyen B, Bix G and Yao Y: Basal lamina changes in neurodegenerative disorders. Mol Neurodegener. 16:812021. View Article : Google Scholar : PubMed/NCBI | |
|
Armulik A, Genové G, Mäe M, Nisancioglu MH, Wallgard E, Niaudet C, He L, Norlin J, Lindblom P, Strittmatter K, et al: Pericytes regulate the blood-brain barrier. Nature. 468:557–561. 2010. View Article : Google Scholar : PubMed/NCBI | |
|
Gaceb A, Özen I, Padel T, Barbariga M and Paul G: Pericytes secrete pro-regenerative molecules in response to platelet-derived growth factor-BB. J Cereb Blood Flow Metab. 38:45–57. 2018. View Article : Google Scholar : | |
|
Dabravolski SA, Andreeva ER, Eremin II, Markin AM, Nadelyaeva II, Orekhov AN and Melnichenko AA: The role of pericytes in regulation of innate and adaptive immunity. Biomedicines. 11:6002023. View Article : Google Scholar : PubMed/NCBI | |
|
Giovannoni F and Quintana FJ: The role of astrocytes in CNS inflammation. Trends Immunol. 41:805–819. 2020. View Article : Google Scholar : PubMed/NCBI | |
|
Abbott NJ, Rönnbäck L and Hansson E: Astrocyte-endothelial interactions at the blood-brain barrier. Nat Rev Neurosci. 7:41–53. 2006. View Article : Google Scholar | |
|
Díaz-Castro B, Robel S and Mishra A: Astrocyte endfeet in brain function and pathology: Open questions. Annu Rev Neurosci. 46:101–121. 2023. View Article : Google Scholar : PubMed/NCBI | |
|
Alvarez JI, Dodelet-Devillers A, Kebir H, Ifergan I, Fabre PJ, Terouz S, Sabbagh M, Wosik K, Bourbonnière L, Bernard M, et al: The hedgehog pathway promotes blood-brain barrier integrity and CNS immune quiescence. Science. 334:1727–1731. 2011. View Article : Google Scholar : PubMed/NCBI | |
|
Xing G, Zhao T, Zhang X, Li H, Li X, Cui P, Li M, Li D, Zhang N and Jiang W: Astrocytic Sonic hedgehog alleviates intracerebral hemorrhagic brain injury via modulation of blood-brain barrier integrity. Front Cell Neurosci. 14:5756902020. View Article : Google Scholar : PubMed/NCBI | |
|
Takahashi S: Metabolic contribution and cerebral blood flow regulation by astrocytes in the neurovascular unit. Cells. 11:8132022. View Article : Google Scholar : PubMed/NCBI | |
|
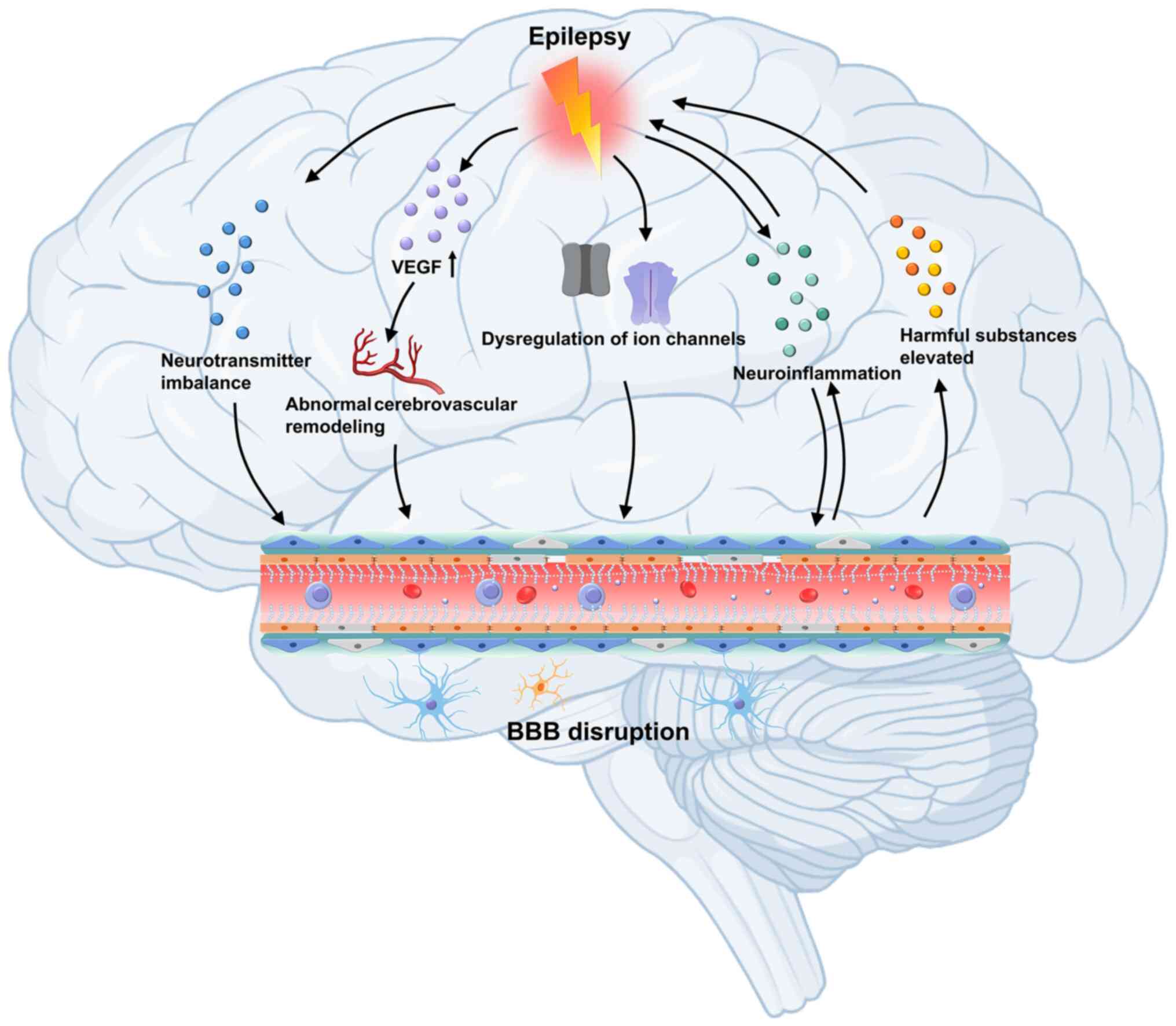
Cornford EM and Oldendorf WH: Epilepsy and the blood-brain barrier. Adv Neurol. 44:787–812. 1986.PubMed/NCBI | |
|
Leroy C, Roch C, Koning E, Namer IJ and Nehlig A: In the lithium-pilocarpine model of epilepsy, brain lesions are not linked to changes in blood-brain barrier permeability: An autoradiographic study in adult and developing rats. Exp Neurol. 182:361–372. 2003. View Article : Google Scholar : PubMed/NCBI | |
|
Saija A, Princi P, Pisani A, Santoro G, De Pasquale R, Massi M and Costa G: Blood-brain barrier dysfunctions following systemic injection of kainic acid in the rat. Life Sci. 51:467–477. 1992. View Article : Google Scholar : PubMed/NCBI | |
|
Librizzi L, Noè F, Vezzani A, de Curtis M and Ravizza T: Seizure-induced brain-borne inflammation sustains seizure recurrence and blood-brain barrier damage. Ann Neurol. 72:82–90. 2012. View Article : Google Scholar : PubMed/NCBI | |
|
Michalak Z, Sano T, Engel T, Miller-Delaney SFC, Lerner-Natoli M and Henshall DC: Spatio-temporally restricted blood-brain barrier disruption after intra-amygdala kainic acid-induced status epilepticus in mice. Epilepsy Res. 103:167–179. 2013. View Article : Google Scholar | |
|
Löscher W: Epilepsy and alterations of the blood-brain barrier: Cause or consequence of epileptic seizures or both? Handb Exp Pharmacol. 273:331–350. 2022. View Article : Google Scholar | |
|
Castañeda-Cabral JL, Colunga-Durán A, Ureña-Guerrero ME, Beas-Zárate C, Nuñez-Lumbreras MLA, Orozco-Suárez S, Alonso-Vanegas M, Guevara-Guzmán R, Deli MA, Valle-Dorado MG, et al: Expression of VEGF- and tight junction-related proteins in the neocortical microvasculature of patients with drug-resistant temporal lobe epilepsy. Microvasc Res. 132:1040592020. View Article : Google Scholar : PubMed/NCBI | |
|
Morin-Brureau M, Lebrun A, Rousset MC, Fagni L, Bockaert J, de Bock F and Lerner-Natoli M: Epileptiform activity induces vascular remodeling and zonula occludens 1 downregulation in organotypic hippocampal cultures: Role of VEGF signaling pathways. J Neurosci. 31:10677–10688. 2011. View Article : Google Scholar : PubMed/NCBI | |
|
Rempe RG, Hartz AMS, Soldner ELB, Sokola BS, Alluri SR, Abner EL, Kryscio RJ, Pekcec A, Schlichtiger J and Bauer B: Matrix metalloproteinase-mediated blood-brain barrier dysfunction in epilepsy. J Neurosci. 38:4301–4315. 2018. View Article : Google Scholar : PubMed/NCBI | |
|
Bronisz E, Cudna A, Wierzbicka A and Kurkowska-Jastrzębska I: Blood-brain barrier-associated proteins are elevated in serum of epilepsy patients. Cells. 12:3682023. View Article : Google Scholar : PubMed/NCBI | |
|
Lai M, Zou W, Han Z, Zhou L, Qiu Z, Chen J, Zhang S, Lai P, Li K, Zhang Y, et al: Tsc1 regulates tight junction independent of mTORC1. Proc Natl Acad Sci USA. 118:e20208911182021. View Article : Google Scholar : PubMed/NCBI | |
|
Guo D, Zhang B, Han L, Rensing NR and Wong M: Cerebral vascular and blood brain-barrier abnormalities in a mouse model of epilepsy and tuberous sclerosis complex. Epilepsia. 65:483–496. 2024. View Article : Google Scholar : | |
|
Ogaki A, Ikegaya Y and Koyama R: Vascular abnormalities and the role of vascular endothelial growth factor in the epileptic brain. Front Pharmacol. 11:202020. View Article : Google Scholar : PubMed/NCBI | |
|
Sweeney MD, Zhao Z, Montagne A, Nelson AR and Zlokovic BV: Blood-brain barrier: From physiology to disease and back. Physiol Rev. 99:21–78. 2019. View Article : Google Scholar : | |
|
Klement W, Blaquiere M, Zub E, deBock F, Boux F, Barbier E, Audinat E, Lerner-Natoli M and Marchi N: A pericyte-glia scarring develops at the leaky capillaries in the hippocampus during seizure activity. Epilepsia. 60:1399–1411. 2019. View Article : Google Scholar : PubMed/NCBI | |
|
Prager O, Kamintsky L, Hasam-Henderson LA, Schoknecht K, Wuntke V, Papageorgiou I, Swolinsky J, Muoio V, Bar-Klein G, Vazana U, et al: Seizure-induced microvascular injury is associated with impaired neurovascular coupling and blood-brain barrier dysfunction. Epilepsia. 60:322–336. 2019. View Article : Google Scholar : PubMed/NCBI | |
|
Li Q, Li QQ, Jia JN, Liu ZQ, Zhou HH and Mao XY: Targeting gap junction in epilepsy: Perspectives and challenges. Biomed Pharmacother. 109:57–65. 2019. View Article : Google Scholar | |
|
Haruwaka K, Ikegami A, Tachibana Y, Ohno N, Konishi H, Hashimoto A, Matsumoto M, Kato D, Ono R, Kiyama H, et al: Dual microglia effects on blood brain barrier permeability induced by systemic inflammation. Nat Commun. 10:58162019. View Article : Google Scholar : PubMed/NCBI | |
|
Park H, Choi SH, Kong MJ and Kang TC: Dysfunction of 67-kDa laminin receptor disrupts bbb integrity via impaired dystrophin/AQP4 complex and p38 MAPK/VEGF activation following status epilepticus. Front Cell Neurosci. 13:2362019. View Article : Google Scholar : PubMed/NCBI | |
|
Zhu H, Dai R, Zhou Y, Fu H and Meng Q: TLR2 ligand Pam3CSK4 regulates MMP-2/9 expression by MAPK/NF-κB signaling pathways in primary brain microvascular endothelial cells. Neurochem Res. 43:1897–1904. 2018. View Article : Google Scholar : PubMed/NCBI | |
|
Yazarlou F, Lipovich L and Loeb JA: Emerging roles of long non-coding RNAs in human epilepsy. Epilepsia. 65:1491–1511. 2024. View Article : Google Scholar : PubMed/NCBI | |
|
Du Y, Chi X and An W: Downregulation of microRNA-200c-3p reduces damage of hippocampal neurons in epileptic rats by upregulating expression of RECK and inactivating the AKT signaling pathway. Chem Biol Interact. 307:223–233. 2019. View Article : Google Scholar : PubMed/NCBI | |
|
Meijer WC and Gorter JA: Role of blood-brain barrier dysfunction in the development of poststroke epilepsy. Epilepsia. 65:2519–2536. 2024. View Article : Google Scholar : PubMed/NCBI | |
|
Ngo A, Royer J, Rodriguez-Cruces R, Xie K, DeKraker J, Auer H, Tavakol S, Lam J, Schrader DV, Dudley RWR, et al: Associations of cerebral blood flow patterns with gray and white matter structure in patients with temporal lobe epilepsy. Neurology. 103:e2095282024. View Article : Google Scholar : PubMed/NCBI | |
|
Musaeus CS, Kjaer TW, Lindberg U, Vestergaard MB, Bo H, Larsson W, Press DZ, Andersen BB, Høgh P, Kidmose P, et al: Subclinical epileptiform discharges in Alzheimer's disease are associated with increased hippocampal blood flow. Alzheimers Res Ther. 16:802024. View Article : Google Scholar : PubMed/NCBI | |
|
Chai AB, Callaghan R and Gelissen IC: Regulation of P-glycoprotein in the brain. Int J Mol Sci. 23:146672022. View Article : Google Scholar : PubMed/NCBI | |
|
Tishler DM, Weinberg KI, Hinton DR, Barbaro N, Annett GM and Raffel C: MDR1 gene expression in brain of patients with medically intractable epilepsy. Epilepsia. 36:1–6. 1995. View Article : Google Scholar : PubMed/NCBI | |
|
Lazarowski A, Ramos AJ, García-Rivello H, Brusco A and Girardi E: Neuronal and glial expression of the multidrug resistance gene product in an experimental epilepsy model. Cell Mol Neurobiol. 24:77–85. 2004. View Article : Google Scholar : PubMed/NCBI | |
|
Hartz AMS, Pekcec A, Soldner ELB, Zhong Y, Schlichtiger J and Bauer B: P-gp protein expression and transport activity in rodent seizure models and human epilepsy. Mol Pharm. 14:999–1011. 2017. View Article : Google Scholar : PubMed/NCBI | |
|
Liu JYW, Thom M, Catarino CB, Mar tinian L, Figarella-Branger D, Bartolomei F, Koepp M and Sisodiya SM: Neuropathology of the blood-brain barrier and pharmaco-resistance in human epilepsy. Brain. 135:3115–3133. 2012. View Article : Google Scholar : PubMed/NCBI | |
|
van Vliet EA, Redeker S, Aronica E, Edelbroek PM and Gorter JA: Expression of multidrug transporters MRP1, MRP2, and BCRP shortly after status epilepticus, during the latent period, and in chronic epileptic rats. Epilepsia. 46:1569–1580. 2005. View Article : Google Scholar : PubMed/NCBI | |
|
Aronica E, Gorter JA, Redeker S, van Vliet EA, Ramkema M, Scheffer GL, Scheper RJ, van der Valk P, Leenstra S, Baayen JC, et al: Localization of breast cancer resistance protein (BCRP) in microvessel endothelium of human control and epileptic brain. Epilepsia. 46:849–857. 2005. View Article : Google Scholar : PubMed/NCBI | |
|
Aronica E, Gorter JA, Jansen GH, van Veelen CW, van Rijen PC, Leenstra S, Ramkema M, Scheffer GL, Scheper RJ and Troost D: Expression and cellular distribution of multidrug transporter proteins in two major causes of medically intractable epilepsy: Focal cortical dysplasia and glioneuronal tumors. Neuroscience. 118:417–429. 2003. View Article : Google Scholar : PubMed/NCBI | |
|
Ferreira A, Rodrigues M, Fortuna A, Falcão A and Alves G: Flavonoid compounds as reversing agents of the P-glycoprotein-mediated multidrug resistance: An in vitro evaluation with focus on antiepileptic drugs. Food Res Int. 103:110–120. 2018. View Article : Google Scholar : PubMed/NCBI | |
|
Gil-Martins E, Barbosa DJ, Silva V, Remião F and Silva R: Dysfunction of ABC transporters at the blood-brain barrier: Role in neurological disorders. Pharmacol Ther. 213:1075542020. View Article : Google Scholar : PubMed/NCBI | |
|
Vijay N and Morris ME: Role of monocarboxylate transporters in drug delivery to the brain. Curr Pharm Des. 20:1487–1498. 2014. View Article : Google Scholar : | |
|
Lauritzen F, Perez EL, Melillo ER, Roh JM, Zaveri HP, Lee TS, Wang Y, Bergersen LH and Eid T: Altered expression of brain monocarboxylate transporter 1 in models of temporal lobe epilepsy. Neurobiol Dis. 45:165–176. 2012. View Article : Google Scholar : | |
|
van Vliet EA, Otte WM, Gorter JA, Dijkhuizen RM and Wadman WJ: Longitudinal assessment of blood-brain barrier leakage during epileptogenesis in rats. A quantitative MRI study Neurobiol Dis. 63:74–84. 2014. View Article : Google Scholar | |
|
Bar-Klein G, Lublinsky S, Kamintsky L, Noyman I, Veksler R, Dalipaj H, Senatorov VV Jr, Swissa E, Rosenbach D, Elazary N, et al: Imaging blood-brain barrier dysfunction as a biomarker for epileptogenesis. Brain. 140:1692–1705. 2017. View Article : Google Scholar : PubMed/NCBI | |
|
Scott G, Mahmud M, Owen DR and Johnson MR: Microglial positron emission tomography (PET) imaging in epilepsy: Applications, opportunities and pitfalls. Seizure. 44:42–47. 2017. View Article : Google Scholar | |
|
Gruenbaum BF, Zlotnik A, Fleidervish I, Frenkel A and Boyko M: Glutamate neurotoxicity and destruction of the blood-brain barrier: Key pathways for the development of neuropsychiatric consequences of TBI and their potential treatment strategies. Int J Mol Sci. 23:96282022. View Article : Google Scholar : PubMed/NCBI | |
|
Barker-Haliski M and White HS: Glutamatergic mechanisms associated with seizures and epilepsy. Cold Spring Harb Perspect Med. 5:a0228632015. View Article : Google Scholar : PubMed/NCBI | |
|
Hogan-Cann AD and Anderson CM: Physiological roles of non-neuronal NMDA receptors. Trends Pharmacol Sci. 37:750–767. 2016. View Article : Google Scholar : PubMed/NCBI | |
|
Kim KS, Jeon MT, Kim ES, Lee CH and Kim DG: Activation of NMDA receptors in brain endothelial cells increases transcellular permeability. Fluids Barriers CNS. 19:702022. View Article : Google Scholar : PubMed/NCBI | |
|
Sharp CD, Hines I, Houghton J, Warren A, Jackson TH IV, Jawahar A, Nanda A, Elrod JW, Long A, Chi A, et al: Glutamate causes a loss in human cerebral endothelial barrier integrity through activation of NMDA receptor. Am J Physiol Heart Circ Physiol. 285:H2592–H2598. 2003. View Article : Google Scholar : PubMed/NCBI | |
|
Chen JT, Chen TG, Chang YC, Chen CY and Chen RM: Roles of NMDARs in maintenance of the mouse cerebrovascular endothelial cell-constructed tight junction barrier. Toxicology. 339:40–50. 2016. View Article : Google Scholar | |
|
Yang T, Liu YW, Zhao L, Wang H, Yang N, Dai SS and He F: Metabotropic glutamate receptor 5 deficiency inhibits neutrophil infiltration after traumatic brain injury in mice. Sci Rep. 7:99982017. View Article : Google Scholar : PubMed/NCBI | |
|
Ren J, Yang T, Liu H, Ma P, Zhou M, Li J, Li T, Sun J, He W, Xu L, et al: Metabotropic glutamate receptor 5 promotes blood-brain barrier recovery after traumatic brain injury. Exp Neurol. 374:1146912024. View Article : Google Scholar : PubMed/NCBI | |
|
Liu J, Feng X, Wang Y, Xia X and Zheng JC: Astrocytes: GABAceptive and GABAergic cells in the brain. Front Cell Neurosci. 16:8924972022. View Article : Google Scholar : PubMed/NCBI | |
|
Kopeikina E, Dukhinova M, Yung AWY, Veremeyko T, Kuznetsova IS, Lau TYB, Levchuk K and Ponomarev ED: Platelets promote epileptic seizures by modulating brain serotonin level, enhancing neuronal electric activity, and contributing to neuroinflammation and oxidative stress. Prog Neurobiol. 188:1017832020. View Article : Google Scholar : PubMed/NCBI | |
|
Wang Y, Zhu Y, Wang J, Dong L, Liu S, Li S and Wu Q: Purinergic signaling: A gatekeeper of blood-brain barrier permeation. Front Pharmacol. 14:11127582023. View Article : Google Scholar : PubMed/NCBI | |
|
Zhao H, Zhang X, Dai Z, Feng Y, Li Q, Zhang JH, Liu X, Chen Y and Feng H: P2X7 receptor suppression preserves blood-brain barrier through inhibiting RhoA activation after experimental intracerebral hemorrhage in rats. Sci Rep. 6:232862016. View Article : Google Scholar : PubMed/NCBI | |
|
Wang K, Sun M, Juan Z, Zhang J, Sun Y, Wang G, Wang C, Li Y, Kong W, Fan L, et al: The improvement of sepsis-associated encephalopathy by P2X7R inhibitor through inhibiting the Omi/HtrA2 apoptotic signaling pathway. Behav Neurol. 2022:37773512022. View Article : Google Scholar : PubMed/NCBI | |
|
van Vliet EA, Otte WM, Wadman WJ, Aronica E, Kooij G, de Vries HE, Dijkhuizen RM and Gorter JA: Blood-brain barrier leakage after status epilepticus in rapamycin-treated rats II: Potential mechanisms. Epilepsia. 57:70–78. 2016. View Article : Google Scholar | |
|
Feng L, Shu Y, Wu Q, Liu T, Long H, Yang H, Li Y and Xiao B: EphA4 may contribute to microvessel remodeling in the hippocampal CA1 and CA3 areas in a mouse model of temporal lobe epilepsy. Mol Med Rep. 15:37–46. 2017. View Article : Google Scholar : | |
|
Rigau V, Morin M, Rousset MC, de Bock F, Lebrun A, Coubes P, Picot MC, Baldy-Moulinier M, Bockaert J, Crespel A and Lerner-Natoli M: Angiogenesis is associated with blood-brain barrier permeability in temporal lobe epilepsy. Brain. 130:1942–1956. 2007. View Article : Google Scholar : PubMed/NCBI | |
|
Hoeben A, Landuyt B, Highley MS, Wildiers H, Van Oosterom AT and De Bruijn EA: Vascular endothelial growth factor and angiogenesis. Pharmacol Rev. 56:549–580. 2004. View Article : Google Scholar : PubMed/NCBI | |
|
Waldbaum S and Patel M: Mitochondrial dysfunction and oxidative stress: A contributing link to acquired epilepsy? J Bioenerg Biomembr. 42:449–455. 2010. View Article : Google Scholar : PubMed/NCBI | |
|
Pugh CW and Ratcliffe PJ: Regulation of angiogenesis by hypoxia: Role of the HIF system. Nat Med. 9:677–684. 2003. View Article : Google Scholar : PubMed/NCBI | |
|
Marchi N, Granata T, Ghosh C and Janigro D: Blood-brain barrier dysfunction and epilepsy: Pathophysiologic role and therapeutic approaches. Epilepsia. 53:1877–1886. 2012. View Article : Google Scholar : PubMed/NCBI | |
|
Wengert ER and Patel MK: The role of the persistent sodium current in epilepsy. Epilepsy Curr. 21:40–47. 2021. View Article : Google Scholar : | |
|
Di Cristo G, Awad PN, Hamidi S and Avoli M: KCC2, epileptiform synchronization, and epileptic disorders. Prog Neurobiol. 162:1–16. 2018. View Article : Google Scholar | |
|
Xu JH and Tang FR: Voltage-dependent calcium channels, calcium binding proteins, and their interaction in the pathological process of epilepsy. Int J Mol Sci. 19:27352018. View Article : Google Scholar : PubMed/NCBI | |
|
Dalal PJ, Muller WA and Sullivan DP: Endothelial cell calcium signaling during barrier function and inflammation. Am J Pathol. 190:535–542. 2020. View Article : Google Scholar : | |
|
Wu J, Yang J, Yu M, Sun W, Han Y, Lu X, Jin C, Wu S and Cai Y: Lanthanum chloride causes blood-brain barrier disruption through intracellular calcium-mediated RhoA/Rho kinase signaling and myosin light chain kinase. Metallomics. 12:2075–2083. 2020. View Article : Google Scholar : PubMed/NCBI | |
|
Luh C, Feiler S, Frauenknecht K, Meyer S, Lubomirov LT, Neulen A and Thal SC: The contractile apparatus is essential for the integrity of the blood-brain barrier after experimental subarachnoid hemorrhage. Transl Stroke Res. 10:534–545. 2019. View Article : Google Scholar : | |
|
Hubbard JA, Szu JI, Yonan JM and Binder DK: Regulation of astrocyte glutamate transporter-1 (GLT1) and aquaporin-4 (AQP4) expression in a model of epilepsy. Exp Neurol. 283:85–96. 2016. View Article : Google Scholar : PubMed/NCBI | |
|
Alvestad S, Hammer J, Hoddevik EH, Skare Ø, Sonnewald U, Amiry-Moghaddam M and Ottersen OP: Mislocalization of AQP4 precedes chronic seizures in the kainate model of temporal lobe epilepsy. Epilepsy Res. 105:30–41. 2013. View Article : Google Scholar : PubMed/NCBI | |
|
Salman MM, Sheilabi MA, Bhattacharyya D, Kitchen P, Conner AC, Bill RM, Woodroofe MN, Conner MT and Princivalle AP: Transcriptome analysis suggests a role for the differential expression of cerebral aquaporins and the MAPK signalling pathway in human temporal lobe epilepsy. Eur J Neurosci. 46:2121–2132. 2017. View Article : Google Scholar : PubMed/NCBI | |
|
Vandebroek A and Yasui M: Regulation of AQP4 in the central nervous system. Int J Mol Sci. 21:16032020. View Article : Google Scholar : PubMed/NCBI | |
|
Bonosi L, Benigno UE, Musso S, Giardina K, Gerardi RM, Brunasso L, Costanzo R, Paolini F, Buscemi F, Avallone C, et al: The role of aquaporins in epileptogenesis-a systematic review. Int J Mol Sci. 24:119232023. View Article : Google Scholar : PubMed/NCBI | |
|
Zhu DD, Yang G, Huang YL, Zhang T, Sui AR, Li N, Su WH, Sun HL, Gao JJ, Ntim M, et al: AQP4-A25Q point mutation in mice depolymerizes orthogonal arrays of particles and decreases polarized expression of AQP4 protein in astrocytic endfeet at the blood-brain barrier. J Neurosci. 42:8169–8183. 2022. View Article : Google Scholar : PubMed/NCBI | |
|
Lin X, Peng Y, Guo Z, He W, Guo W, Feng J, Lu L, Liu Q and Xu P: Short-chain fatty acids suppresses astrocyte activation by amplifying Trp-AhR-AQP4 signaling in experimental autoimmune encephalomyelitis mice. Cell Mol Life Sci. 81:2932024. View Article : Google Scholar : PubMed/NCBI | |
|
Lee DJ, Hsu MS, Seldin MM, Arellano JL and Binder DK: Decreased expression of the glial water channel aquaporin-4 in the intrahippocampal kainic acid model of epileptogenesis. Exp Neurol. 235:246–255. 2012. View Article : Google Scholar : PubMed/NCBI | |
|
Murphy TR, Davila D, Cuvelier N, Young LR, Lauderdale K, Binder DK and Fiacco TA: Hippocampal and cortical pyramidal neurons swell in parallel with astrocytes during acute hypoosmolar stress. Front Cell Neurosci. 11:2752017. View Article : Google Scholar : PubMed/NCBI | |
|
Seiffert E, Dreier JP, Ivens S, Bechmann I, Tomkins O, Heinemann U and Friedman A: Lasting blood-brain barrier disruption induces epileptic focus in the rat somatosensory cortex. J Neurosci. 24:7829–7836. 2004. View Article : Google Scholar : PubMed/NCBI | |
|
van Vliet EA, da Costa Araújo S, Redeker S, van Schaik R, Aronica E and Gorter JA: Blood-brain barrier leakage may lead to progression of temporal lobe epilepsy. Brain. 130:521–534. 2007. View Article : Google Scholar | |
|
Savotchenko A, Klymenko M, Shypshyna M and Isaev D: The role of thrombin in early-onset seizures. Front Cell Neurosci. 17:11010062023. View Article : Google Scholar : PubMed/NCBI | |
|
Greene C, Hanley N, Reschke CR, Reddy A, Mäe MA, Connolly R, Behan C, O'Keeffe E, Bolger I, Hudson N, et al: Microvascular stabilization via blood-brain barrier regulation prevents seizure activity. Nat Commun. 13:20032022. View Article : Google Scholar | |
|
Liu XX, Yang L, Shao LX, He Y, Wu G, Bao YH, Lu NN, Gong DM, Lu YP, Cui TT, et al: Endothelial Cdk5 deficit leads to the development of spontaneous epilepsy through CXCL1/CXCR2-mediated reactive astrogliosis. J Exp Med. 217:e201809922020. View Article : Google Scholar : | |
|
Salar S, Maslarova A, Lippmann K, Nichtweiss J, Weissberg I, Sheintuch L, Kunz WS, Shorer Z, Friedman A and Heinemann U: Blood-brain barrier dysfunction can contribute to pharmacoresistance of seizures. Epilepsia. 55:1255–1263. 2014. View Article : Google Scholar : PubMed/NCBI | |
|
Lapilover EG, Lippmann K, Salar S, Maslarova A, Dreier JP, Heinemann U and Friedman A: Peri-infarct blood-brain barrier dysfunction facilitates induction of spreading depolarization associated with epileptiform discharges. Neurobiol Dis. 48:495–506. 2012. View Article : Google Scholar : PubMed/NCBI | |
|
Frigerio F, Frasca A, Weissberg I, Parrella S, Friedman A, Vezzani A and Noé FM: Long-lasting pro-ictogenic effects induced in vivo by rat brain exposure to serum albumin in the absence of concomitant pathology. Epilepsia. 53:1887–1897. 2012. View Article : Google Scholar : PubMed/NCBI | |
|
Salar S, Lapilover E, Müller J, Hollnagel JO, Lippmann K, Friedman A and Heinemann U: Synaptic plasticity in area CA1 of rat hippocampal slices following intraventricular application of albumin. Neurobiol Dis. 91:155–165. 2016. View Article : Google Scholar : PubMed/NCBI | |
|
Noé FM, Bellistri E, Colciaghi F, Cipelletti B, Battaglia G, de Curtis M and Librizzi L: Kainic acid-induced albumin leak across the blood-brain barrier facilitates epileptiform hyperexcitability in limbic regions. Epilepsia. 57:967–976. 2016. View Article : Google Scholar : PubMed/NCBI | |
|
Kinboshi M, Ikeda A and Ohno Y: Role of astrocytic inwardly rectifying potassium (Kir) 4.1 channels in epileptogenesis. Front Neurol. 11:6266582020. View Article : Google Scholar | |
|
Szu JI and Binder DK: Mechanisms underlying aquaporin-4 subcellular mislocalization in epilepsy. Front Cell Neurosci. 16:9005882022. View Article : Google Scholar : PubMed/NCBI | |
|
David Y, Cacheaux LP, Ivens S, Lapilover E, Heinemann U, Kaufer D and Friedman A: Astrocytic dysfunction in epileptogenesis: Consequence of altered potassium and glutamate homeostasis? J Neurosci. 29:10588–10599. 2009. View Article : Google Scholar : PubMed/NCBI | |
|
Wallraff A, Köhling R, Heinemann U, Theis M, Willecke K and Steinhäuser C: The impact of astrocytic gap junctional coupling on potassium buffering in the hippocampus. J Neurosci. 26:5438–5447. 2006. View Article : Google Scholar : PubMed/NCBI | |
|
Vezzani A, Ravizza T, Bedner P, Aronica E, Steinhäuser C and Boison D: Astrocytes in the initiation and progression of epilepsy. Nat Rev Neurol. 18:707–722. 2022. View Article : Google Scholar : PubMed/NCBI | |
|
Qiu YM, Zhang CL, Chen AQ, Wang HL, Zhou YF, Li YN and Hu B: Immune cells in the BBB disruption after acute ischemic stroke: Targets for immune therapy? Front Immunol. 12:6787442021. View Article : Google Scholar : PubMed/NCBI | |
|
Yang J, Ran M, Li H, Lin Y, Ma K, Yang Y, Fu X and Yang S: New insight into neurological degeneration: Inflammatory cytokines and blood-brain barrier. Front Mol Neurosci. 15:10139332022. View Article : Google Scholar : PubMed/NCBI | |
|
Broekaart DWM, Anink JJ, Baayen JC, Idema S, de Vries HE, Aronica E, Gorter JA and van Vliet EA: Activation of the innate immune system is evident throughout epileptogenesis and is associated with blood-brain barrier dysfunction and seizure progression. Epilepsia. 59:1931–1944. 2018. View Article : Google Scholar : PubMed/NCBI | |
|
Di Nunzio M, Di Sapia R, Sorrentino D, Kebede V, Cerovic M, Gullotta GS, Bacigaluppi M, Audinat E, Marchi N, Ravizza T and Vezzani A: Microglia proliferation plays distinct roles in acquired epilepsy depending on disease stages. Epilepsia. 62:1931–1945. 2021. View Article : Google Scholar : PubMed/NCBI | |
|
Kamaşak T, Dilber B, Yaman SÖ, Durgut BD, Kurt T, Çoban E, Arslan EA, Şahin S, Karahan SC and Cansu A: HMGB-1, TLR4, IL-1R1, TNF-α, and IL-1β: Novel epilepsy markers? Epileptic Disord. 22:183–193. 2020. View Article : Google Scholar | |
|
Greene C, Hanley N and Campbell M: Claudin-5: Gatekeeper of neurological function. Fluids Barriers CNS. 16:32019. View Article : Google Scholar : PubMed/NCBI | |
|
Clark PR, Kim RK, Pober JS and Kluger MS: Tumor necrosis factor disrupts claudin-5 endothelial tight junction barriers in two distinct NF-κB-dependent phases. PLoS One. 10:e01200752015. View Article : Google Scholar | |
|
Khan A, Ni W, Lopez-Giraldez F, Kluger MS, Pober JS and Pierce RW: Tumor necrosis factor-induced ArhGEF10 selectively activates RhoB contributing to human microvascular endothelial cell tight junction disruption. FASEB J. 35:e216272021. View Article : Google Scholar : PubMed/NCBI | |
|
Tsai MM, Chen JL, Lee TH, Liu H, Shanmugam V and Hsieh HL: Brain protective effect of resveratrol via ameliorating interleukin-1β-induced MMP-9-mediated disruption of ZO-1 arranged integrity. Biomedicines. 10:12702022. View Article : Google Scholar | |
|
Manu DR, Slevin M, Barcutean L, Forro T, Boghitoiu T and Balasa R: Astrocyte involvement in blood-brain barrier function: A critical update highlighting novel, complex, neurovascular interactions. Int J Mol Sci. 24:171462023. View Article : Google Scholar : PubMed/NCBI | |
|
Viviani B, Bartesaghi S, Gardoni F, Vezzani A, Behrens MM, Bartfai T, Binaglia M, Corsini E, Di Luca M, Galli CL and Marinovich M: Interleukin-1beta enhances NMDA receptor-mediated intracellular calcium increase through activation of the Src family of kinases. J Neurosci. 23:8692–8700. 2003. View Article : Google Scholar : PubMed/NCBI | |
|
Mukhtar I: Inflammatory and immune mechanisms underlying epileptogenesis and epilepsy: From pathogenesis to treatment target. Seizure. 82:65–79. 2020. View Article : Google Scholar : PubMed/NCBI | |
|
Yang F, Zhao K, Zhang X, Zhang J and Xu B: ATP induces disruption of tight junction proteins via IL-1 beta-dependent MMP-9 activation of human blood-brain barrier in vitro. Neural Plast. 2016:89285302016. View Article : Google Scholar : PubMed/NCBI | |
|
Qiu J, Xu J, Zheng Y, Wei Y, Zhu X, Lo EH, Moskowitz MA and Sims JR: High-mobility group box 1 promotes metalloproteinase-9 upregulation through Toll-like receptor 4 after cerebral ischemia. Stroke. 41:2077–2082. 2010. View Article : Google Scholar : PubMed/NCBI | |
|
Kim EJ, Park SY, Baek SE, Jang MA, Lee WS, Bae SS, Kim K and Kim CD: HMGB1 Increases IL-1β production in vascular smooth muscle cells via NLRP3 inflammasome. Front Physiol. 9:3132018. View Article : Google Scholar | |
|
de Jong JM, Broekaart DWM, Bongaarts A, Mühlebner A, Mills JD, van Vliet EA and Aronica E: Altered extracellular matrix as an alternative risk factor for epileptogenicity in brain tumors. Biomedicines. 10:24752022. View Article : Google Scholar : PubMed/NCBI | |
|
Su J, Yin J, Qin W, Sha S, Xu J and Jiang C: Role for pro-inflammatory cytokines in regulating expression of GABA transporter type 1 and 3 in specific brain regions of kainic acid-induced status epilepticus. Neurochem Res. 40:621–627. 2015. View Article : Google Scholar : PubMed/NCBI | |
|
Fu CY, He XY, Li XF, Zhang X, Huang ZW, Li J, Chen M and Duan CZ: Nefiracetam attenuates pro-inflammatory cytokines and GABA transporter in specific brain regions of rats with post-ischemic seizures. Cell Physiol Biochem. 37:2023–2031. 2015. View Article : Google Scholar : PubMed/NCBI | |
|
Olmos G and Lladó J: Tumor necrosis factor alpha: A link between neuroinflammation and excitotoxicity. Mediators Inflamm. 2014:8612312014. View Article : Google Scholar : PubMed/NCBI | |
|
Roseti C, van Vliet EA, Cifelli P, Ruffolo G, Baayen JC, Di Castro MA, Bertollini C, Limatola C, Aronica E, Vezzani A and Palma E: GABAA currents are decreased by IL-1β in epileptogenic tissue of patients with temporal lobe epilepsy: Implications for ictogenesis. Neurobiol Dis. 82:311–320. 2015. View Article : Google Scholar : PubMed/NCBI | |
|
Librizzi L, Vila Verde D, Colciaghi F, Deleo F, Regondi MC, Costanza M, Cipelletti B and de Curtis M: Peripheral blood mononuclear cell activation sustains seizure activity. Epilepsia. 62:1715–1728. 2021. View Article : Google Scholar : PubMed/NCBI | |
|
Cresto N, Janvier A and Marchi N: From neurons to the neuro-glio-vascular unit: Seizures and brain homeostasis in networks. Rev Neurol (Paris). 179:308–315. 2023. View Article : Google Scholar : PubMed/NCBI | |
|
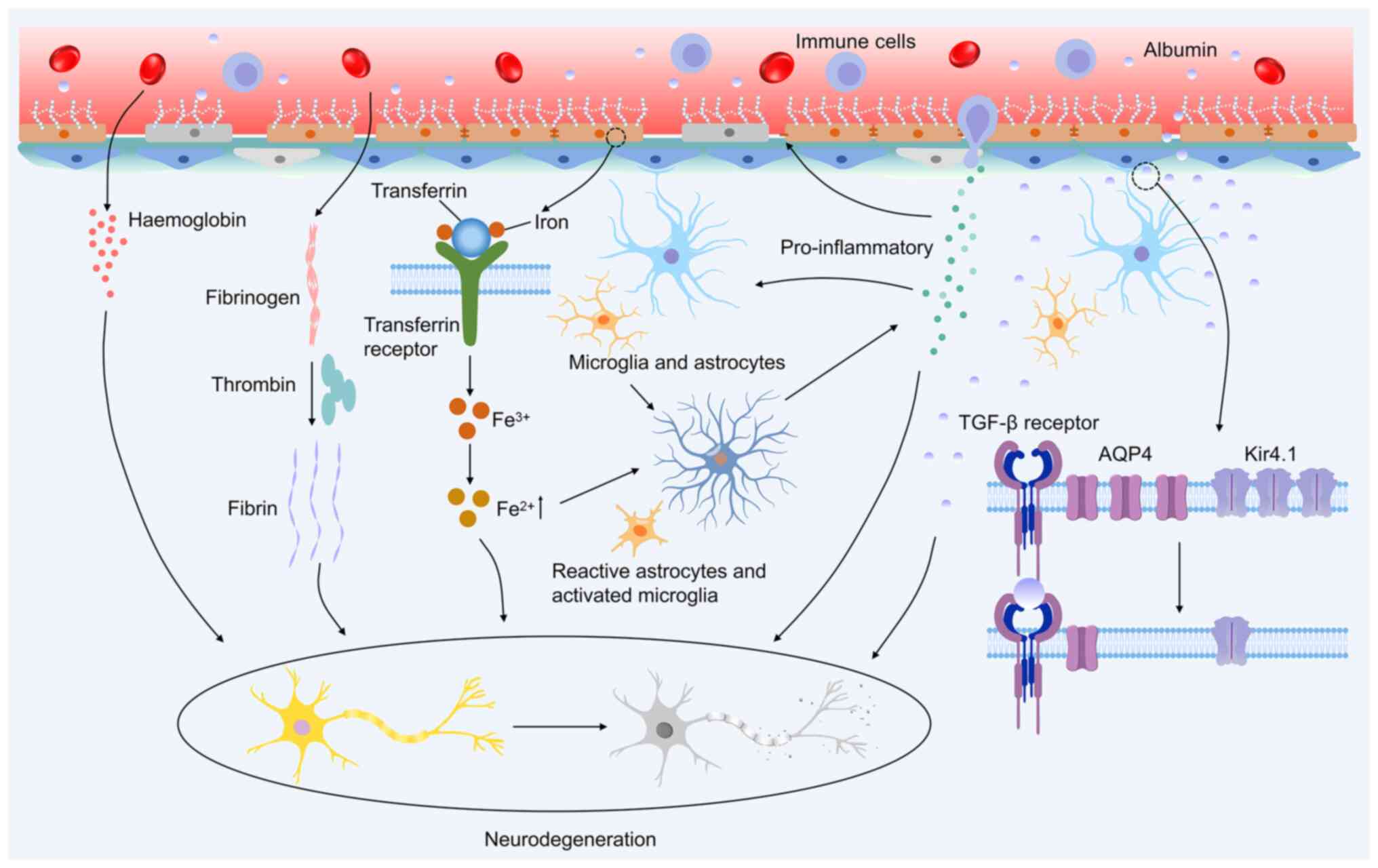
Thirupathi A and Chang YZ: Brain iron metabolism and CNS diseases. Adv Exp Med Biol. 1173:1–19. 2019. View Article : Google Scholar : PubMed/NCBI | |
|
Tang S, Gao P, Chen H, Zhou X, Ou Y and He Y: The role of iron, its metabolism and ferroptosis in traumatic brain injury. Front Cell Neurosci. 14:5907892020. View Article : Google Scholar : PubMed/NCBI | |
|
Chiueh CC: Iron overload, oxidative stress, and axonal dystrophy in brain disorders. Pediatr Neurol. 25:138–147. 2001. View Article : Google Scholar : PubMed/NCBI | |
|
Willmore LJ, Sypert GW and Munson JB: Recurrent seizures induced by cortical iron injection: a model of posttraumatic epilepsy. Ann Neurol. 4:329–336. 1978. View Article : Google Scholar : PubMed/NCBI | |
|
Willmore LJ, Sypert GW, Munson JV and Hurd RW: Chronic focal epileptiform discharges induced by injection of iron into rat and cat cortex. Science. 200:1501–1503. 1978. View Article : Google Scholar : PubMed/NCBI | |
|
Zimmer TS, David B, Broekaart DWM, Schidlowski M, Ruffolo G, Korotkov A, van der Wel NN, van Rijen PC, Mühlebner A, van Hecke W, et al: Seizure-mediated iron accumulation and dysregulated iron metabolism after status epilepticus and in temporal lobe epilepsy. Acta Neuropathol. 142:729–759. 2021. View Article : Google Scholar : PubMed/NCBI | |
|
Ikeda M: Iron overload without the C282Y mutation in patients with epilepsy. J Neurol Neurosurg Psychiatry. 70:551–553. 2001. View Article : Google Scholar : PubMed/NCBI | |
|
Dusek P, Hofer T, Alexander J, Roos PM and Aaseth JO: Cerebral iron deposition in neurodegeneration. Biomolecules. 12:7142022. View Article : Google Scholar : PubMed/NCBI | |
|
Bagwe-Parab S and Kaur G: Molecular targets and therapeutic interventions for iron induced neurodegeneration. Brain Res Bull. 156:1–9. 2020. View Article : Google Scholar | |
|
Wang F, Guo L, Wu Z, Zhang T, Dong D and Wu B: The Clock gene regulates kainic acid-induced seizures through inhibiting ferroptosis in mice. J Pharm Pharmacol. 74:1640–1650. 2022. View Article : Google Scholar : PubMed/NCBI | |
|
Mao XY, Zhou HH and Jin WL: Ferroptosis induction in pentylenetetrazole kindling and pilocarpine-induced epileptic seizures in mice. Front Neurosci. 13:7212019. View Article : Google Scholar : PubMed/NCBI | |
|
Huang L, Liu H and Liu S: Insight into the role of ferroptosis in epilepsy. J Integr Neurosci. 23:1132024. View Article : Google Scholar : PubMed/NCBI | |
|
Vezzani A, French J, Bartfai T and Baram TZ: The role of inflammation in epilepsy. Nat Rev Neurol. 7:31–40. 2011. View Article : Google Scholar | |
|
Montagne A, Zhao Z and Zlokovic BV: Alzheimer's disease: A matter of blood-brain barrier dysfunction? J Exp Med. 214:3151–3169. 2017. View Article : Google Scholar : PubMed/NCBI | |
|
Profaci CP, Munji RN, Pulido RS and Daneman R: The blood-brain barrier in health and disease: Important unanswered questions. J Exp Med. 217:e201900622020. View Article : Google Scholar : PubMed/NCBI | |
|
Lendahl U, Nilsson P and Betsholtz C: Emerging links between cerebrovascular and neurodegenerative diseases-a special role for pericytes. EMBO Rep. 20:e480702019. View Article : Google Scholar | |
|
Bell RD, Winkler EA, Sagare AP, Singh I, LaRue B, Deane R and Zlokovic BV: Pericytes control key neurovascular functions and neuronal phenotype in the adult brain and during brain aging. Neuron. 68:409–427. 2010. View Article : Google Scholar : PubMed/NCBI | |
|
Davalos D, Ryu JK, Merlini M, Baeten KM, Le Moan N, Petersen MA, Deerinck TJ, Smirnoff DS, Bedard C, Hakozaki H, et al: Fibrinogen-induced perivascular microglial clustering is required for the development of axonal damage in neuroinflammation. Nat Commun. 3:12272012. View Article : Google Scholar : PubMed/NCBI | |
|
Marchi N, Angelov L, Masaryk T, Fazio V, Granata T, Hernandez N, Hallene K, Diglaw T, Franic L, Najm I and Janigro D: Seizure-promoting effect of blood-brain barrier disruption. Epilepsia. 48:732–742. 2007. View Article : Google Scholar : PubMed/NCBI | |
|
Oby E and Janigro D: The blood-brain barrier and epilepsy. Epilepsia. 47:1761–1774. 2006. View Article : Google Scholar : PubMed/NCBI | |
|
van Vliet EA, Ndode-Ekane XE, Lehto LJ, Gorter JA, Andrade P, Aronica E, Gröhn O and Pitkänen A: Long-lasting blood-brain barrier dysfunction and neuroinflammation after traumatic brain injury. Neurobiol Dis. 145:1050802020. View Article : Google Scholar : PubMed/NCBI | |
|
Zhao Y, Liu Y, Xu Y, Li K, Zhou L, Qiao H, Xu Q and Zhao J: The role of ferroptosis in blood-brain barrier injury. Cell Mol Neurobiol. 43:223–236. 2023. View Article : Google Scholar | |
|
Yang LT, Anthony G and Kaufer D: Inflammatory astrocytic TGFβ signaling induced by blood-brain barrier dysfunction drives epileptogenesis. Noebels JL, Avoli M, Rogawski MA, Vezzani A and Delgado-Escueta AV: Jasper's Basic Mechanisms of the Epilepsies. 5th edition. New York: Oxford University Press; 2024 | |
|
van Vliet EA, Aronica E and Gorter JA: Blood-brain barrier dysfunction, seizures and epilepsy. Semin Cell Dev Biol. 38:26–34. 2015. View Article : Google Scholar | |
|
Belinskaia DA, Voronina PA, Shmurak VI, Jenkins RO and Goncharov NV: Serum albumin in health and disease: Esterase, antioxidant, transporting and signaling properties. Int J Mol Sci. 22:103182021. View Article : Google Scholar : PubMed/NCBI | |
|
Wang Y: Leaky blood-brain barrier: A double whammy for the brain. Epilepsy Currents. 20:165–167. 2020. View Article : Google Scholar : PubMed/NCBI | |
|
Luo WD, Min JW, Huang WX, Wang X, Peng YY, Han S, Yin J, Liu WH, He XH and Peng BW: Vitexin reduces epilepsy after hypoxic ischemia in the neonatal brain via inhibition of NKCC1. J Neuroinflammation. 15:1862018. View Article : Google Scholar : PubMed/NCBI | |
|
Ahishali B, Kaya M, Orhan N, Arican N, Ekizoglu O, Elmas I, Kucuk M, Kemikler G, Kalayci R and Gurses C: Effects of levetiracetam on blood-brain barrier disturbances following hyperthermia-induced seizures in rats with cortical dysplasia. Life Sci. 87:609–619. 2010. View Article : Google Scholar : PubMed/NCBI | |
|
Shaikh TG, Hasan SFS, Ahmed H, Kazi AI and Mansoor R: The role of angiotensin receptor blockers in treating epilepsy: A review. Neurol Sci. 45:1437–1445. 2024. View Article : Google Scholar | |
|
Rodriguez-Ortiz CJ, Thorwald MA, Rodriguez R, Mejias-Ortega M, Kieu Z, Maitra N, Hawkins C, Valenzuela J, Peng M, Nishiyama A, et al: Angiotensin receptor blockade with olmesartan alleviates brain pathology in obese OLETF rats. Clin Exp Pharmacol Physiol. 50:228–237. 2023. View Article : Google Scholar : | |
|
Pereira MGAG, Becari C, Oliveira JAC, Salgado MCO, Garcia-Cairasco N and Costa-Neto CM: Inhibition of the renin-angiotensin system prevents seizures in a rat model of epilepsy. Clin Sci (Lond). 119:477–482. 2010. View Article : Google Scholar : PubMed/NCBI | |
|
Winkler EA, Sengillo JD, Sagare AP, Zhao Z, Ma Q, Zuniga E, Wang Y, Zhong Z, Sullivan JS, Griffin JH, et al: Blood-spinal cord barrier disruption contributes to early motor-neuron degeneration in ALS-model mice. Proc Natl Acad Sci USA. 111:E1035–E1042. 2014. View Article : Google Scholar : PubMed/NCBI | |
|
Cui J, Liu X and Chow LMC: Flavonoids as P-gp inhibitors: A systematic review of SARs. Curr Med Chem. 26:4799–4831. 2019. View Article : Google Scholar | |
|
Deng X, Shao Y, Xie Y, Feng Y, Wu M, Wang M and Chen Y: MicroRNA-146a-5p downregulates the expression of P-glycoprotein in rats with lithium-pilocarpine-induced status epilepticus. Biol Pharm Bull. 42:744–750. 2019. View Article : Google Scholar : PubMed/NCBI | |
|
Merelli A, Ramos AJ, Lazarowski A and Auzmendi J: Convulsive stress mimics brain hypoxia and promotes the P-glycoprotein (P-gp) and erythropoietin receptor overexpression. Recombinant human erythropoietin effect on P-gp activity. Front Neurosci. 13:7502019. View Article : Google Scholar : PubMed/NCBI | |
|
Montanari F and Ecker GF: Prediction of drug-ABC-transporter interaction-recent advances and future challenges. Adv Drug Deliv Rev. 86:17–26. 2015. View Article : Google Scholar : PubMed/NCBI | |
|
Yu J and Ragueneau-Majlessi I: In Vitro-to-in vivo extrapolation of transporter inhibition data for drugs approved by the US food and drug administration in 2018. Clin Transl Sci. 13:693–699. 2020. View Article : Google Scholar : PubMed/NCBI | |
|
Faal T, Phan DTT, Davtyan H, Scarfone VM, Varady E, Blurton-Jones M, Hughes CCW and Inlay MA: Induction of mesoderm and neural crest-derived pericytes from human pluripotent stem cells to study blood-brain barrier interactions. Stem Cell Reports. 12:451–460. 2019. View Article : Google Scholar : PubMed/NCBI | |
|
Chen B: Cell therapy rejuvenates the neuroglial-vascular unit. Neural Regen Res. 21: View Article : Google Scholar : 2025. | |
|
Dahalia M, Gupta S, Majid H, Vohora D and Nidhi: Pirfenidone regulates seizures through the HMGB1/TLR4 axis to improve cognitive functions and modulate oxidative stress and neurotransmitters in PTZ-induced kindling in mice. Front Pharmacol. 15:15280322025. View Article : Google Scholar : PubMed/NCBI | |
|
Wang Q, Qin B, Yu H, Yu H, Zhang X, Li M, Zhou Y, Diao L and Liu H: Dingxian pill alleviates hippocampal neuronal apoptosis in epileptic mice through TNF-α/TNFR1 signaling pathway inhibition. J Ethnopharmacol. 334:1185792024. View Article : Google Scholar | |
|
Chen S, Chen R, Luo M, Luo Y, Ma X, Zhao H and Xu Z: Increased seizure susceptibility in the collagen-induced arthritis mouse model depends on neuronal IL-1R1. Life Sci. 369:1235372025. View Article : Google Scholar : PubMed/NCBI | |
|
Wu L, Zhu Y, Qin Y, Yuan H, Zhang L, Lu T, Chen Q and Hu A: Conditional knockout of IL-1R1 in endothelial cells attenuates seizures and neurodegeneration via inhibiting neuroinflammation mediated by Nrf2/HO-1/NLRP3 signaling in status epilepticus model. Mol Neurobiol. 61:4289–4303. 2024. View Article : Google Scholar : | |
|
Walker LE, Sills GJ, Jorgensen A, Alapirtti T, Peltola J, Brodie MJ, Marson AG, Vezzani A and Pirmohamed M: High-mobility group box 1 as a predictive biomarker for drug-resistant epilepsy: A proof-of-concept study. Epilepsia. 63:e1–e6. 2022. View Article : Google Scholar | |
|
Zhao J, Zheng Y, Liu K, Chen J, Lai N, Fei F, Shi J, Xu C, Wang S, Nishibori M, et al: HMGB1 is a therapeutic target and biomarker in diazepam-refractory status epilepticus with wide time window. Neurotherapeutics. 17:710–721. 2020. View Article : Google Scholar : | |
|
Rana A and Musto AE: The role of inflammation in the development of epilepsy. J Neuroinflammation. 15:1442018. View Article : Google Scholar : PubMed/NCBI | |
|
Mariette X, Matucci-Cerinic M, Pavelka K, Taylor P, van Vollenhoven R, Heatley R, Walsh C, Lawson R, Reynolds A and Emery P: Malignancies associated with tumour necrosis factor inhibitors in registries and prospective observational studies: A systematic review and meta-analysis. Ann Rheum Dis. 70:1895–1904. 2011. View Article : Google Scholar : PubMed/NCBI | |
|
Vezzani A, Balosso S and Ravizza T: Neuroinflammatory pathways as treatment targets and biomarkers in epilepsy. Nat Rev Neurol. 15:459–472. 2019. View Article : Google Scholar : PubMed/NCBI | |
|
Ravizza T and Vezzani A: Pharmacological targeting of brain inflammation in epilepsy: Therapeutic perspectives from experimental and clinical studies. Epilepsia Open. 3(Suppl 2): S133–S142. 2018. View Article : Google Scholar | |
|
Soltani Khaboushan A, Yazdanpanah N and Rezaei N: Neuroinflammation and proinflammatory cytokines in epileptogenesis. Mol Neurobiol. 59:1724–1743. 2022. View Article : Google Scholar : PubMed/NCBI | |
|
Dilena R, Mauri E, Aronica E, Bernasconi P, Bana C, Cappelletti C, Carrabba G, Ferrero S, Giorda R, Guez S, et al: Therapeutic effect of Anakinra in the relapsing chronic phase of febrile infection-related epilepsy syndrome. Epilepsia Open. 4:344–350. 2019. View Article : Google Scholar : PubMed/NCBI | |
|
Costagliola G, Depietri G, Michev A, Riva A, Foiadelli T, Savasta S, Bonuccelli A, Peroni D, Consolini R, Marseglia GL, et al: Targeting inflammatory mediators in epilepsy: A systematic review of its molecular basis and clinical applications. Front Neurol. 13:7412442022. View Article : Google Scholar : PubMed/NCBI | |
|
Zhong X, Na Y, Yin S, Yan C, Gu J, Zhang N and Geng F: Cell membrane biomimetic nanoparticles with potential in treatment of Alzheimer's disease. Molecules. 28:23362023. View Article : Google Scholar : PubMed/NCBI | |
|
Qin Y, Fan W, Chen H, Yao N, Tang W, Tang J, Yuan W, Kuai R, Zhang Z, Wu Y and He Q: In vitro and in vivo investigation of glucose-mediated brain-targeting liposomes. J Drug Target. 18:536–549. 2010. View Article : Google Scholar : PubMed/NCBI | |
|
Xie F, Yao N, Qin Y, Zhang Q, Chen H, Yuan M, Tang J, Li X, Fan W, Zhang Q, et al: Investigation of glucose-modified liposomes using polyethylene glycols with different chain lengths as the linkers for brain targeting. Int J Nanomedicine. 7:163–175. 2012. View Article : Google Scholar : PubMed/NCBI | |
|
Zhou Y, Zhu F, Liu Y, Zheng M, Wang Y, Zhang D, Anraku Y, Zou Y, Li J, Wu H, et al: Blood-brain barrier-penetrating siRNA nanomedicine for Alzheimer's disease therapy. Sci Adv. 6:eabc70312020. View Article : Google Scholar : PubMed/NCBI | |
|
Anraku Y, Kuwahara H, Fukusato Y, Mizoguchi A, Ishii T, Nitta K, Matsumoto Y, Toh K, Miyata K, Uchida S, et al: Glycaemic control boosts glucosylated nanocarrier crossing the BBB into the brain. Nat Commun. 8:10012017. View Article : Google Scholar : PubMed/NCBI | |
|
Fu X, Li J, Wu Y, Mao C and Jiang Y: PAR2 deficiency tunes inflammatory microenvironment to magnify STING signalling for mitigating cancer metastasis via anionic CRISPR/Cas9 nanoparticles. J Control Release. 363:733–746. 2023. View Article : Google Scholar : PubMed/NCBI | |
|
Meng R, Hao S, Sun C, Hou Z, Hou Y, Wang L, Deng P, Deng J, Yang Y, Xia H, et al: Reverse-QTY code design of active human serum albumin self-assembled amphiphilic nanoparticles for effective anti-tumor drug doxorubicin release in mice. Proc Natl Acad Sci USA. 120:e22201731202023. View Article : Google Scholar : PubMed/NCBI | |
|
Gu GJ, Chung H, Park JY, Yoo R, Im HJ, Choi H, Lee YS and Seok SH: Mannosylated-serum albumin nanoparticle imaging to monitor tumor-associated macrophages under anti-PD1 treatment. J Nanobiotechnology. 21:312023. View Article : Google Scholar : PubMed/NCBI | |
|
Deng Z, Wang J, Xiao Y, Li F, Niu L, Liu X, Meng L and Zheng H: Ultrasound-mediated augmented exosome release from astrocytes alleviates amyloid-β-induced neurotoxicity. Theranostics. 11:4351–4362. 2021. View Article : Google Scholar : | |
|
Qu F, Wang P, Zhang K, Shi Y, Li Y, Li C, Lu J, Liu Q and Wang X: Manipulation of mitophagy by 'all-in-one' nanosensitizer augments sonodynamic glioma therapy. Autophagy. 16:1413–1435. 2020. View Article : Google Scholar | |
|
Gasca-Salas C, Fernández-Rodríguez B, Pineda-Pardo JA, Rodríguez-Rojas R, Obeso I, Hernández-Fernández F, Del Álamo M, Mata D, Guida P, Ordás-Bandera C, et al: Blood-brain barrier opening with focused ultrasound in Parkinson's disease dementia. Nat Commun. 12:7792021. View Article : Google Scholar : PubMed/NCBI | |
|
Ozdas MS, Shah AS, Johnson PM, Patel N, Marks M, Yasar TB, Stalder U, Bigler L, von der Behrens W, Sirsi SR and Yanik MF: Non-invasive molecularly-specific millimeter-resolution manipulation of brain circuits by ultrasound-mediated aggregation and uncaging of drug carriers. Nat Commun. 11:49292020. View Article : Google Scholar : PubMed/NCBI | |
|
Chen J, Yuan M, Madison CA, Eitan S and Wang Y: Blood-brain barrier crossing using magnetic stimulated nanoparticles. J Control Release. 345:557–571. 2022. View Article : Google Scholar : PubMed/NCBI | |
|
Gupta R, Chauhan A, Kaur T, Kuanr BK and Sharma D: Transmigration of magnetite nanoparticles across the blood-brain barrier in a rodent model: Influence of external and alternating magnetic fields. Nanoscale. 14:17589–17606. 2022. View Article : Google Scholar : PubMed/NCBI | |
|
Zhang Q, Yang L, Zheng Y, Wu X, Chen X, Fei F, Gong Y, Tan B, Chen Q, Wang Y, et al: Electro-responsive micelle-based universal drug delivery system for on-demand therapy in epilepsy. J Control Release. 360:759–771. 2023. View Article : Google Scholar : PubMed/NCBI | |
|
Zhang Y, Wu X, Ding J, Su B, Chen Z, Xiao Z, Wu C, Wei D, Sun J, Luo F, et al: Wireless-powering deep brain stimulation platform based on 1D-structured magnetoelectric nanochains applied in antiepilepsy treatment. ACS Nano. 17:15796–15809. 2023. View Article : Google Scholar : PubMed/NCBI | |
|
Gao S, Zheng M, Ren X, Tang Y and Liang X: Local hyperthermia in head and neck cancer: Mechanism, application and advance. Oncotarget. 7:57367–57378. 2016. View Article : Google Scholar : PubMed/NCBI | |
|
Wu D, Fei F, Zhang Q, Wang X, Gong Y, Chen X, Zheng Y, Tan B, Xu C, Xie H, et al: Nanoengineered on-demand drug delivery system improves efficacy of pharmacotherapy for epilepsy. Sci Adv. 8:eabm33812022. View Article : Google Scholar : PubMed/NCBI | |
|
Yang D, Ren Q, Nie J, Zhang Y, Wu H, Chang Z, Wang B, Dai J and Fang Y: Black phosphorus flake-enabled wireless neuromodulation for epilepsy treatment. Nano Lett. 24:1052–1061. 2024. View Article : Google Scholar | |
|
Hou Q, Wang L, Xiao F, Wang L, Liu X, Zhu L, Lu Y, Zheng W and Jiang X: Dual targeting nanoparticles for epilepsy therapy. Chem Sci. 13:12913–12920. 2022. View Article : Google Scholar : PubMed/NCBI | |
|
Chen SG, Tsai CH, Lin CJ, Lee CC, Yu HY, Hsieh TH and Liu HL: Transcranial focused ultrasound pulsation suppresses pentylenetetrazol induced epilepsy in vivo. Brain Stimul. 13:35–46. 2020. View Article : Google Scholar | |
|
Lee CC, Chou CC, Hsiao FJ, Chen YH, Lin CF, Chen CJ, Peng SJ, Liu HL and Yu HY: Pilot study of focused ultrasound for drug-resistant epilepsy. Epilepsia. 63:162–175. 2022. View Article : Google Scholar | |
|
Gustafson HH, Holt-Casper D, Grainger DW and Ghandehari H: Nanoparticle uptake: The phagocyte problem. Nano Today. 10:487–510. 2015. View Article : Google Scholar : PubMed/NCBI | |
|
Dobrovolskaia MA and McNeil SE: Immunological properties of engineered nanomaterials. Nat Nanotechnol. 2:469–478. 2007. View Article : Google Scholar | |
|
Singh N, Manshian B, Jenkins GJS, Griffiths SM, Williams PM, Maffeis TGG, Wright CJ and Doak SH: NanoGenotoxicology: The DNA damaging potential of engineered nanomaterials. Biomaterials. 30:3891–3914. 2009. View Article : Google Scholar : PubMed/NCBI | |
|
Zhang J, Yan F, Zhang W, He L, Li Y, Zheng S, Wang Y, Yu T, Du L, Shen Y and He W: Biosynthetic gas vesicles combined with focused ultrasound for blood-brain barrier opening. Int J Nanomedicine. 17:6759–6772. 2022. View Article : Google Scholar | |
|
Mainprize T, Lipsman N, Huang Y, Meng Y, Bethune A, Ironside S, Heyn C, Alkins R, Trudeau M, Sahgal A, et al: Blood-brain barrier opening in primary brain tumors with non-invasive MR-guided focused ultrasound: A clinical safety and feasibility study. Sci Rep. 9:3212019. View Article : Google Scholar : PubMed/NCBI | |
|
Lipsman N, Meng Y, Bethune AJ, Huang Y, Lam B, Masellis M, Herrmann N, Heyn C, Aubert I, Boutet A, et al: Blood-brain barrier opening in Alzheimer's disease using MR-guided focused ultrasound. Nat Commun. 9:23362018. View Article : Google Scholar : PubMed/NCBI | |
|
Pineda-Pardo JA, Gasca-Salas C, Fernández-Rodríguez B, Rodríguez-Rojas R, Del Álamo M, Obeso I, Hernández-Fernández F, Trompeta C, Martínez-Fernández R, Matarazzo M, et al: Striatal blood-brain barrier opening in Parkinson's disease dementia: A pilot exploratory study. Mov Disord. 37:2057–2065. 2022. View Article : Google Scholar : PubMed/NCBI | |
|
Gkountas AA, Polychronopoulos ND, Sofiadis GN, Karvelas EG, Spyrou LA and Sarris IE: Simulation of magnetic nanoparticles crossing through a simplified blood-brain barrier model for Glioblastoma multiforme treatment. Comput Methods Programs Biomed. 212:1064772021. View Article : Google Scholar : PubMed/NCBI | |
|
Bencsik A, Lestaevel P and Guseva Canu I: Nano- and neuro-toxicology: An emerging discipline. Prog Neurobiol. 160:45–63. 2018. View Article : Google Scholar | |
|
Xiong X, Sun Y, Sattiraju A, Jung Y, Mintz A, Hayasaka S and Li KC: Remote spatiotemporally controlled and biologically selective permeabilization of blood-brain barrier. J Control Release. 217:113–120. 2015. View Article : Google Scholar : PubMed/NCBI | |
|
Chen W, Yu H, Hao Y, Liu W, Wang R, Huang Y, Wu J, Feng L, Guan Y, Huang L and Qian K: Comprehensive metabolic fingerprints characterize neuromyelitis optica spectrum disorder by nanoparticle-enhanced laser desorption/ionization mass spectrometry. ACS Nano. 17:19779–19792. 2023. View Article : Google Scholar : PubMed/NCBI | |
|
Lyu X, Liu J, Gou Y, Sun S, Hao J and Cui Y: Development and validation of a machine learning-based model of ischemic stroke risk in the Chinese elderly hypertensive population. VIEW. 5:202400592024. View Article : Google Scholar | |
|
Yuan Y, Zhang X, Wang Y, Li H, Qi Z, Du Z, Chu YH, Feng D, Xie Q, Song J, et al: Multimodal data integration using deep learning predicts overall survival of patients with glioma. VIEW. 5:202400012024. View Article : Google Scholar | |
|
Ying X, Wang Y, Liang J, Yue J, Xu C, Lu L, Xu Z, Gao J, Du Y and Chen Z: Angiopep-conjugated electro-responsive hydrogel nanoparticles: Therapeutic potential for epilepsy. Angew Chem Int Ed Engl. 53:12436–12440. 2014. View Article : Google Scholar : PubMed/NCBI | |
|
Geng C, Ren X, Cao P, Chu X, Wei P, Liu Q, Lu Y, Fu B, Li W, Li Y and Zhao G: Macrophage membrane-biomimetic nanoparticles target inflammatory microenvironment for epilepsy treatment. Theranostics. 14:6652–6670. 2024. View Article : Google Scholar : | |
|
Fang Z, Chen S, Qin J, Chen B, Ni G, Chen Z, Zhou J, Li Z, Ning Y, Wu C and Zhou L: Pluronic P85-coated poly(butylcyanoacrylate) nanoparticles overcome phenytoin resistance in P-glycoprotein overexpressing rats with lithium-pilocarpine-induced chronic temporal lobe epilepsy. Biomaterials. 97:110–121. 2016. View Article : Google Scholar : PubMed/NCBI | |
|
Zybina A, Anshakova A, Malinovskaya J, Melnikov P, Baklaushev V, Chekhonin V, Maksimenko O, Titov S, Balabanyan V, Kreuter J, et al: Nanoparticle-based delivery of carbamazepine: A promising approach for the treatment of refractory epilepsy. Int J Pharm. 547:10–23. 2018. View Article : Google Scholar : PubMed/NCBI | |
|
Zhao J, Ye Z, Yang J, Zhang Q, Shan W, Wang X, Wang Z, Ye S, Zhou X, Shao Z and Ren L: Nanocage encapsulation improves antiepileptic efficiency of phenytoin. Biomaterials. 240:1198492020. View Article : Google Scholar : PubMed/NCBI | |
|
Chu PC, Yu HY, Lee CC, Fisher R and Liu HL: Pulsed-focused ultrasound provides long-term suppression of epileptiform bursts in the kainic acid-induced epilepsy rat model. Neurotherapeutics. 19:1368–1380. 2022. View Article : Google Scholar : PubMed/NCBI | |
|
Krishna V, Mindel J, Sammartino F, Block C, Dwivedi AK, Van Gompel JJ, Fountain N and Fisher R: A phase 1 open-label trial evaluating focused ultrasound unilateral anterior thalamotomy for focal onset epilepsy. Epilepsia. 64:831–842. 2023. View Article : Google Scholar : PubMed/NCBI | |
|
Choi T, Koo M, Joo J, Kim T, Shon YM and Park J: Bidirectional neuronal control of epileptiform activity by repetitive transcranial focused ultrasound stimulations. Adv Sci (Weinh). 11:e23024042024. View Article : Google Scholar | |
|
Chu PC, Huang CS, Ing SZ, Yu HY, Fisher RS and Liu HL: Pulsed focused ultrasound reduces hippocampal volume loss and improves behavioral performance in the kainic acid rat model of epilepsy. Neurotherapeutics. 20:502–517. 2023. View Article : Google Scholar : PubMed/NCBI | |
|
Zhang Y, Buckmaster PS, Qiu L, Wang J, Keunen O, Ghobadi SN, Huang A, Hou Q, Li N, Narang S, et al: Non-invasive, neurotoxic surgery reduces seizures in a rat model of temporal lobe epilepsy. Exp Neurol. 343:1137612021. View Article : Google Scholar : PubMed/NCBI | |
|
Zhang M, Li B, Liu Y, Tang R, Lang Y, Huang Q and He J: Different modes of low-frequency focused ultrasound-mediated attenuation of epilepsy based on the topological theory. Micromachines (Basel). 12. pp. 10012021, View Article : Google Scholar |










